Building a barrier
Radiation therapy is a well-established method for treating prostate cancer, targeting the prostate gland to eliminate cancer cells. However, this process has its drawbacks. It can inadvertently affect surrounding tissues, particularly the rectum, which lies close to the prostate, separated only by a thin layer called the rectoprostatic fascia. Despite advances in radiation technology, collateral damage to normal, healthy tissues remains a pesky challenge. Without protective measures, 20–30% of patients experience side effects ranging from increased bowel movement frequency to severe rectal ulcers that may persist for years.
A study conducted at NUH involving 236 patients revealed that 9.3% of them experienced grade 3 rectal bleeding, requiring multiple treatments such as blood transfusions. “The challenge with radiation therapy for prostate cancer has always been how to target the cancer effectively while minimising damage to surrounding tissues, especially the rectum, which is in close proximity to the prostate,” says A/Prof Chiong.
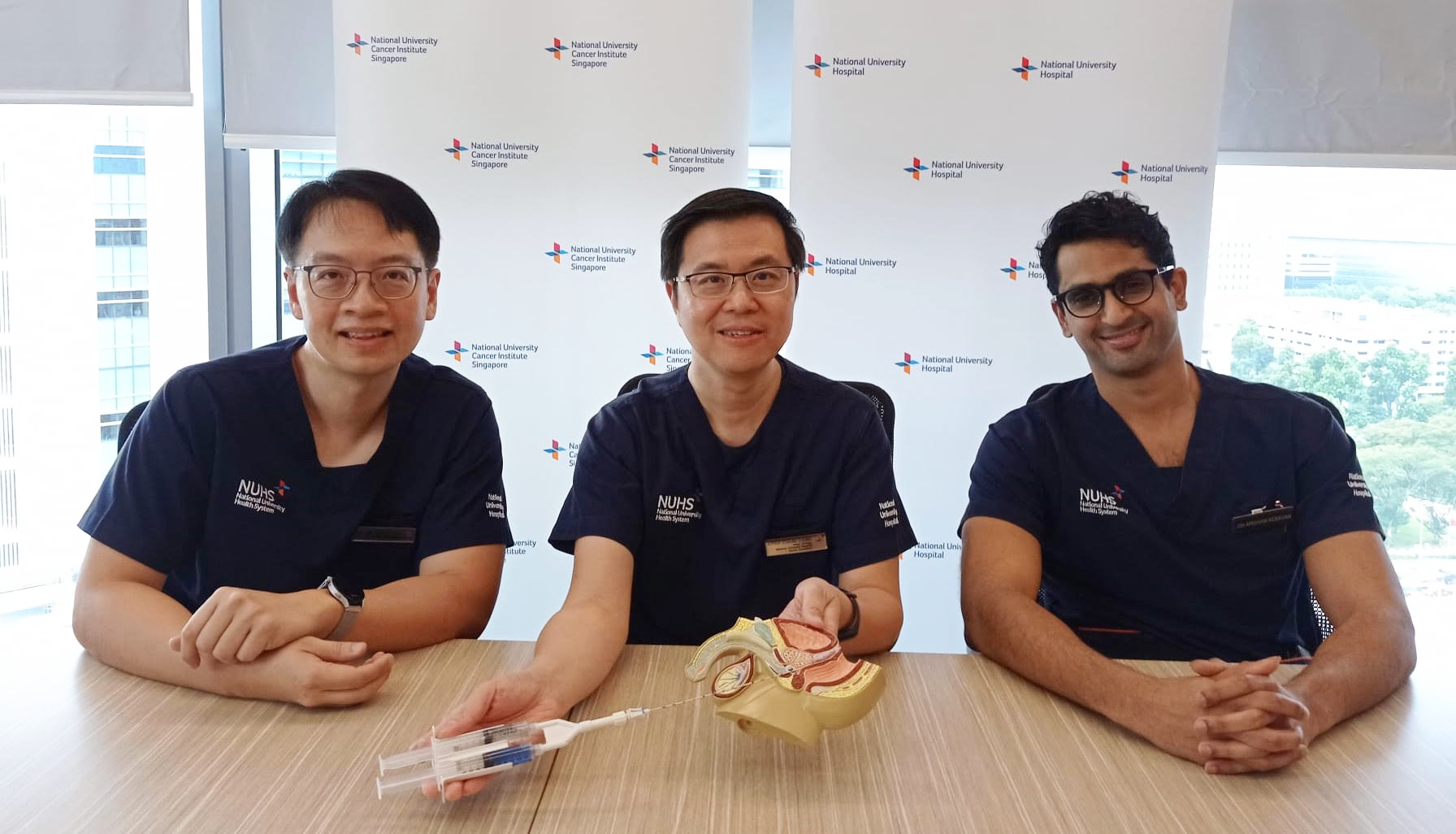
To tackle this issue head-on, doctors at NUH have been using rectal spacers — a gel-like substance inserted into the space between the prostate and rectum. This spacer acts as a physical barrier, inching the rectum away from the high-radiation zone and shielding it from unwanted exposure. The minimally invasive procedure involves injecting the gel through the perineum under general anaesthesia. The entire process takes less than 15 minutes, with patients able to return home the same day.
Tangible benefits
Since its introduction in May 2022, rectal spacers have benefitted more than 150 patients by reducing the side effects of radiation therapy. A follow-up study involving the first 120 patients who underwent the procedure at NUH showed that only 4% experienced minor side effects — a substantial improvement compared to nearly 30% in those who did not use spacers. Inserted two weeks before radiation therapy, the spacers are biodegradable and dissolve in the human body within six to nine months. They are also approved by regulators such as the United States Food and Drug Administration and Singapore’s Health Sciences Authority.
“By adopting this technique, we are not just aiming to treat prostate cancer; we are also focused on enhancing the comfort and improving the quality of life for our patients during and after treatment,” adds A/Prof Chiong.
Each procedure is tailored to each patient, taking into account factors such as tumour size, location and individual anatomy. Patients with locally advanced prostate cancer or those at high risk under general anaesthesia may not qualify for the procedure.
“Our goal is always to provide patient-centred care, tailored to the needs of each individual we treat,” adds Dr Kesavan. “This initiative represents a step forward in providing effective cancer treatment while still preserving good quality of life.”
Like this article? Simply subscribe to make sure you don't miss the next issue of EnvisioningHealth!