Infection Prevention and Control
2025/04/11
Infection prevention and control (IPC) is a practical, evidence-based approach that protects patients and healthcare workers from being harmed by avoidable infections. Effective IPC requires constant effort on all levels of the healthcare system, including policymakers, facility managers, healthcare providers and those who access health services.
Through our ongoing dedication of surveillance, early detection, early isolation, good research and teaching, we hope to shape the future of hand surgery globally.
Why do I need to know about infection?
It’s important for you to understand what an infection is before you learn about the things that might put a person at a higher risk for getting one. An infection occurs when germs enter a person’s body and multiply, causing illness, organ and tissue damage, or disease.
Infection control prevents or stops the spread of infections in healthcare settings.
What is hospital associated infection (HAI)?
Germs are a part of our everyday life. They live in the air, soil, water and in and on our bodies. Some germs are helpful, others are harmful.
Infections are caused by microscopic organisms known as pathogens – bacteria, viruses, fungi, or parasites – that enter the body, multiply, and interfere with normal functions. Only a small portion of germs can cause infection during a hospital stay.
Impact:
HAIs cause sickness and prolong your hospital stay.
Risk:
Healthcare procedures may expose you to germs that cause HAIs. These germs can spread between patients, healthcare providers, staff and visitors through unclean hands and improper use or reuse of equipment.


Preventing infections is in your hands
A few simple precautions can help you avoid getting sick with an infectious disease:
- Washing your hands often with soap and water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitiser.
- Avoid touching your face, mouth, nose, or eyes.
- Cough or sneeze into a tissue, sleeve, or elbow instead of into your hand or into the air. Throw tissue away immediately and wash your hands.
- Do not share personal items, such as razors, toothbrushes, deodorant, combs, brushes and towels with other patients.

Why is hand hygiene important?
Regular handwashing is one of the best ways to remove germs, avoid getting sick, and prevent the spread of germs to others. Germs from unwashed hands can be transferred from objects like handrails, table tops, or toys, to another person’s hands. Therefore, good hand hygiene helps prevent diarrhea and respiratory infections and even skin and eye infections.
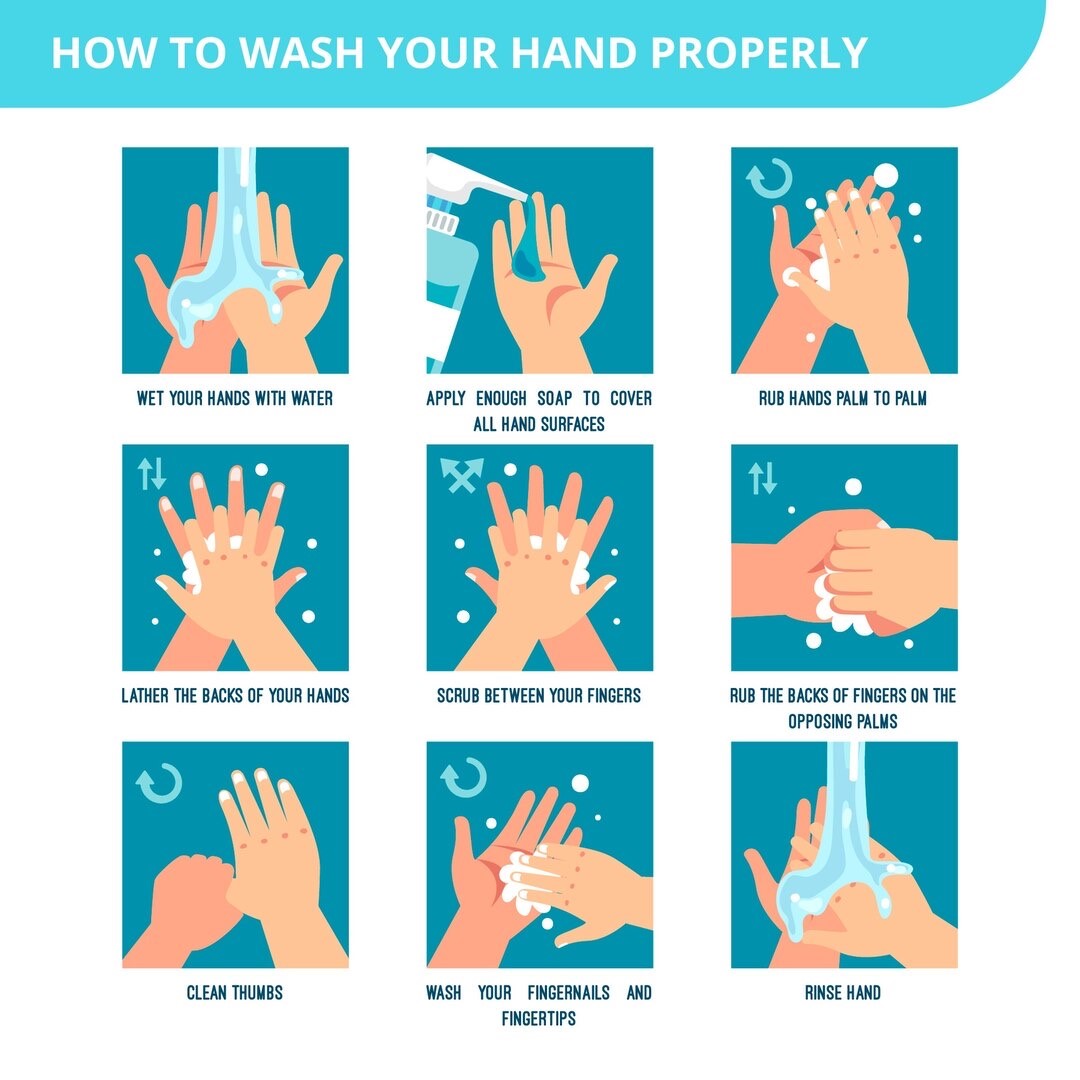
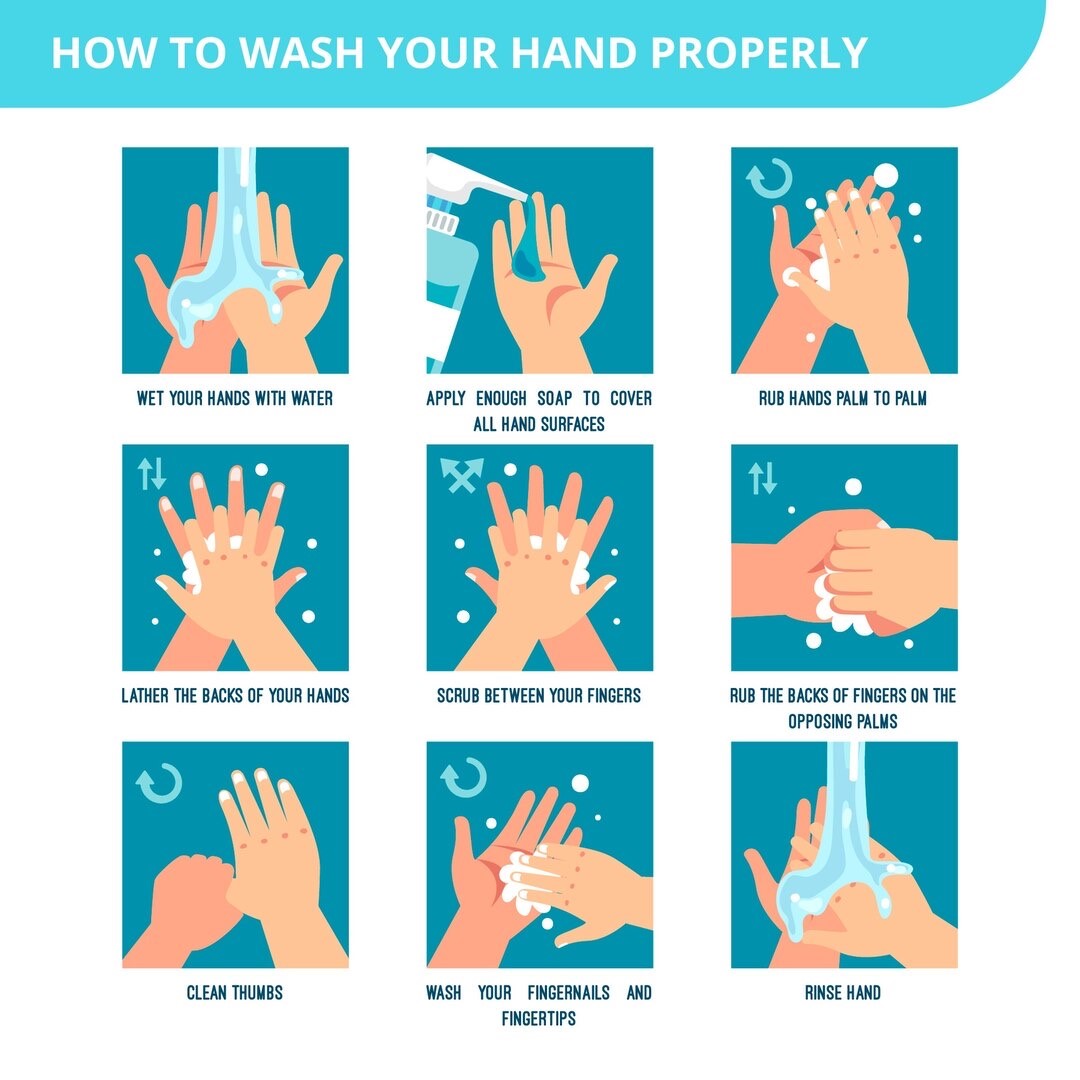
How do you perform hand hygiene?
- Use soap and water
- Use alcohol-based hand rub
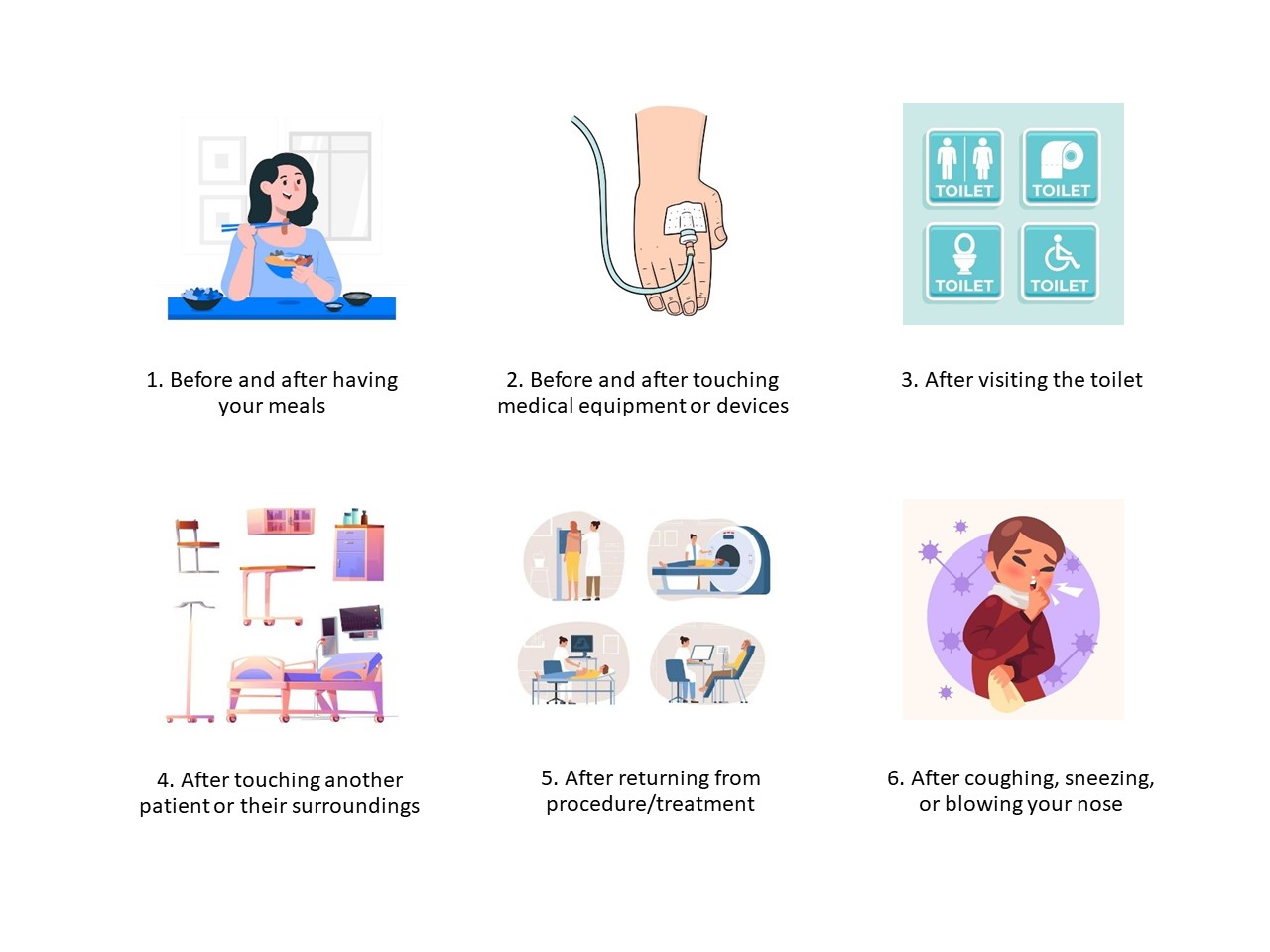
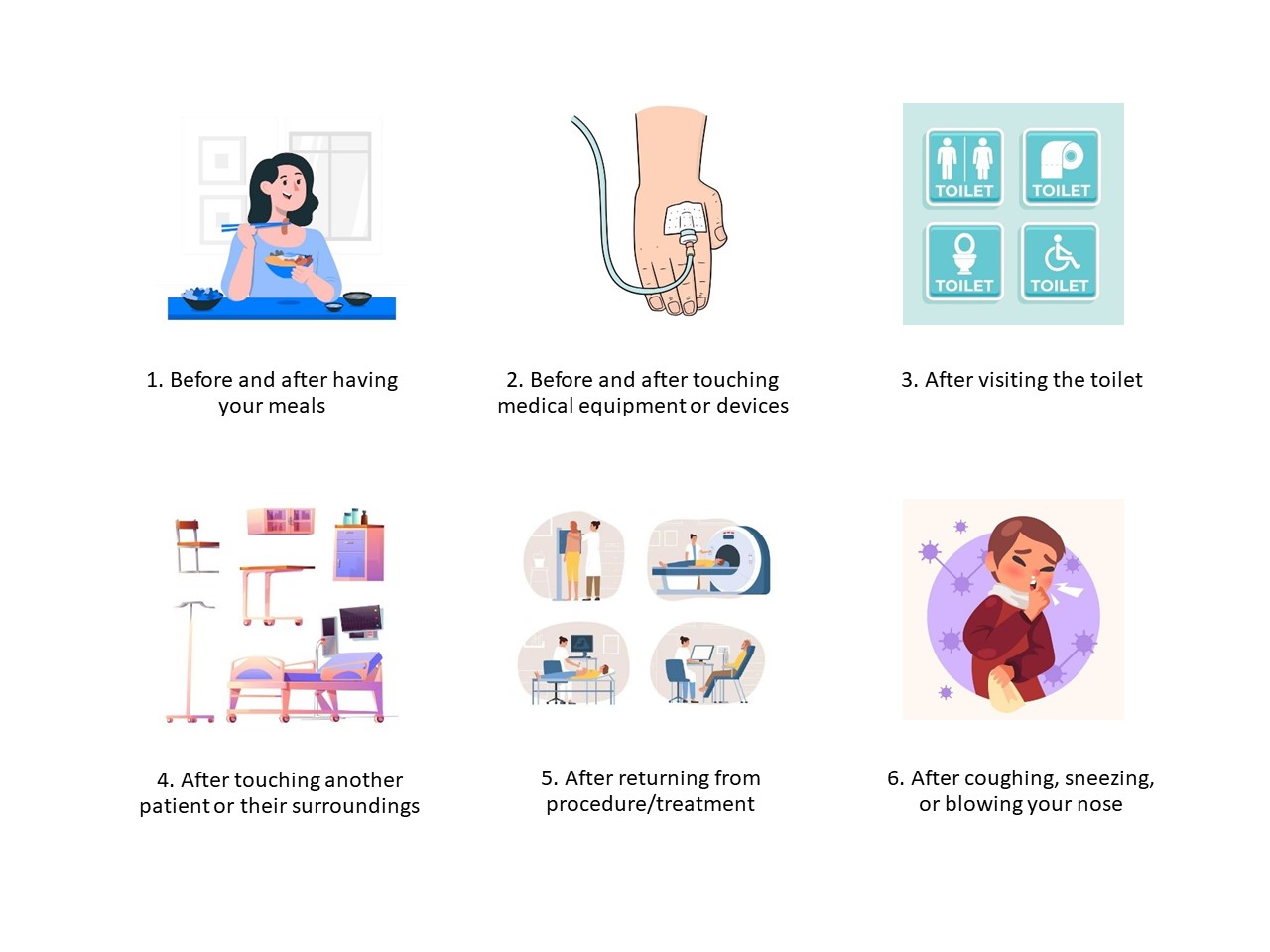
When to perform hand hygiene?


Cough and sneeze etiquette
Infections can easily spread when you have a respiratory infection. Coughing and sneezing can transmit germs to others through the air or by contaminating nearby surfaces. Therefore, it is crucial to adhere to the steps below to effectively prevent the spread of infection:
- Cover your mouth and nose when coughing or sneezing and dispose tissues after use
- Wash your hands / use alcohol-based hand rub after coughing, sneezing or blowing your nose
- Wear a mask when you are near others or when you leave the ward, and remember to keep a safe distance
Multidrug Resistant Organisms (MDROs) are defined as microorganisms that are resistant to several classes of antimicrobials. These bacteria can cause infections with limited treatment options.
Read more about the different MRDOs in the section below.
In our hospital, isolation precautions are strictly followed to prevent the spread of Multidrug Resistant Organisms (MDROs) among vulnerable patients, many of whom may have severe underlying medical problems and are at increased risk of infection.
Surveillance such as screening for MDROs on admission to hospital is key to reducing the development and spread of infections. Early detection of high-risk patients allows early isolation. This reduces the opportunity for transmission if a patient is colonised or infected. Conducting surveillance to monitor MDRO trends over time also allows the assessment of control measures.
Keeping the environment clean and good hand hygiene practice by all staff, patients and visitors can minimise the risk of widespread transmission.
All staff are required to wear gloves and gowns or aprons when attending to patients, and wash their hands with soap and water or use alcohol gel before entering and upon leaving the room. It is very important that patients wash their hands thoroughly with soap and water after visiting the toilet and before eating (our staff will assist patients if needed). Patients are advised to avoid touching any wounds or medical devices such as intravenous drips or catheters.
Having an MDRO infection will not affect patient’s discharge and they will be discharged home when their general condition allows.
Common Multidrug Resistant Organisms (MDROs)