Primary cancers of the bones
Also known as b one sarcomas, osteosarcomas and chondrosarcomas are the two most common variants. These affect individuals of all ages but in particular people who are in their twenties and sixties.
The challenges in managing these conditions revolve around removal of these tumours in a way that they do not recur and then reconstruct the structure to replace the missing anatomical structure and restore function.
The general approaches to reconstruction can be both biological and prosthetic. In biological solutions, the draw is that one is able to reconstruct the missing structure with biological materials and host bone which has a virtually life-long durability. These methods, however, do result in donor site morbidity and have a relatively high early complication rate.
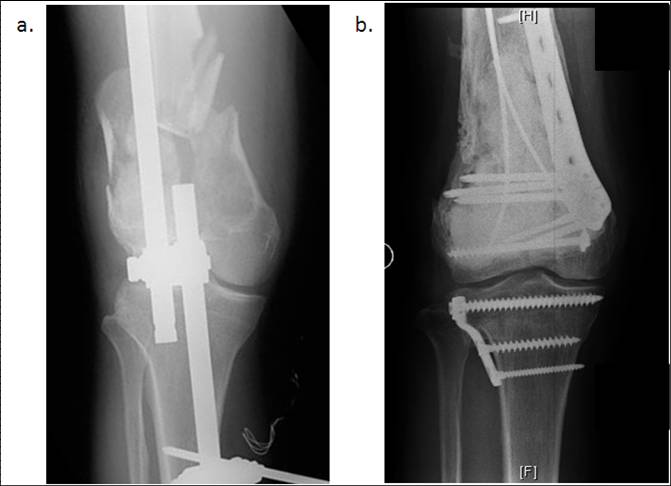
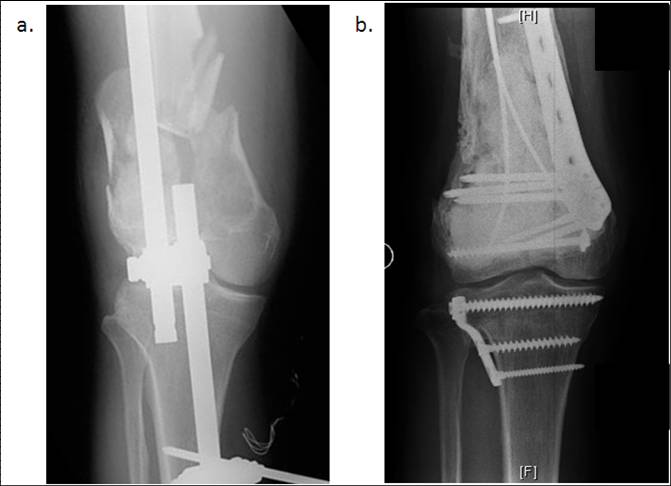
The prosthetic approaches where joints and segments are replaced by metal implants have high patient acceptability and good function but are subject to wear (Figure 1). We have a unique blend of both approaches and hence only the most appropriate is offered in specific cases. Our service has contributed pioneering work in this field with more than thirty years of research in developing novel solutions to the problem. We even have our own in-house bone bank which is the only one of its kind in Singapore and has been responsible for setting up centers regionally.
Primary cancers of the soft tissues
Also known as soft tissue sarcomas, liposarcomas and malignant fibrous histiocytomas more commonly occur in adulthood whereas rhabdomyosarcomas and synovial sarcomas occur in childhood.
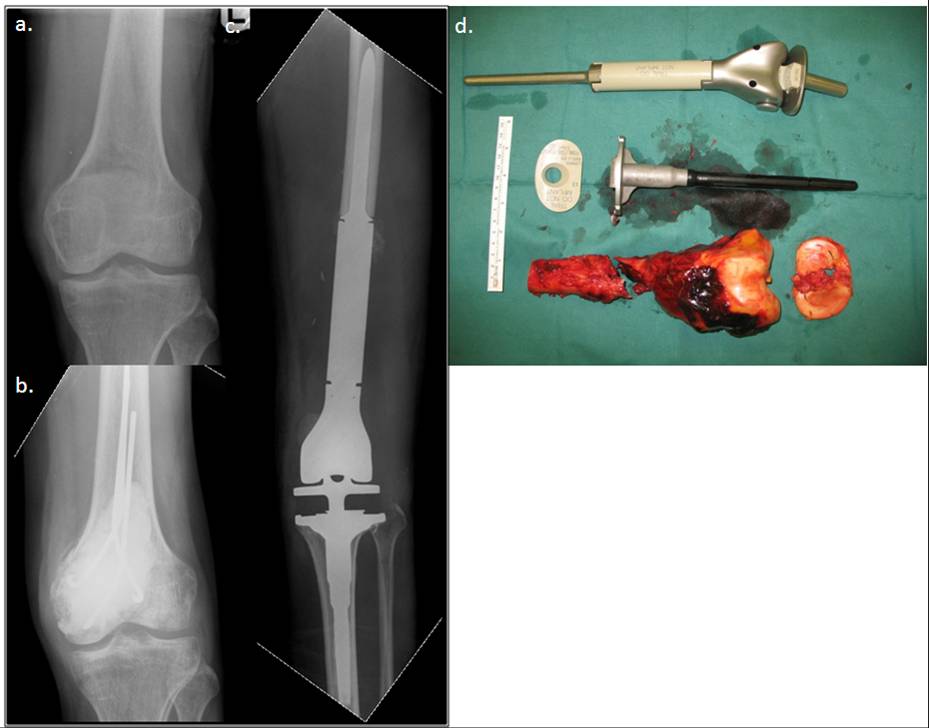
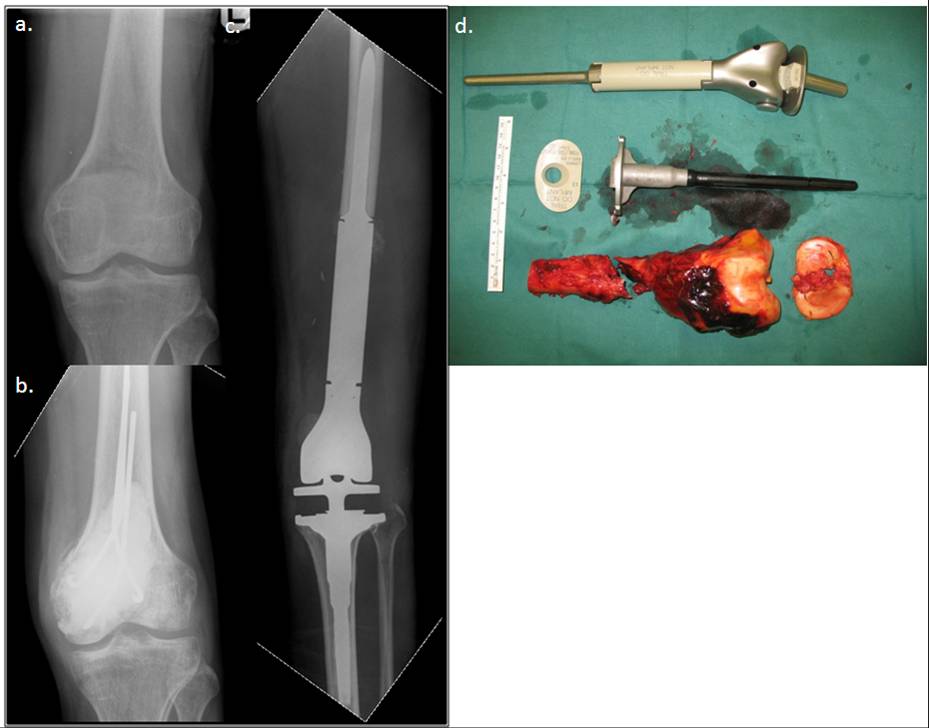
The specific ability of the orthopaedic oncologists is in his ability to resect these tumours primarily to save life and yet secondarily reconstruct defects in a way that maintains function. In addition resections are done in a way that facilitates radiation therapy that is often used in these conditions (Figure 2).
Metastasis
When cancers in other parts of the body spread to the bone and soft tissues, these structures become compromised. As a result patients develop fractures that do not heal and they become invalid. This in turn reduces their life expectancy.
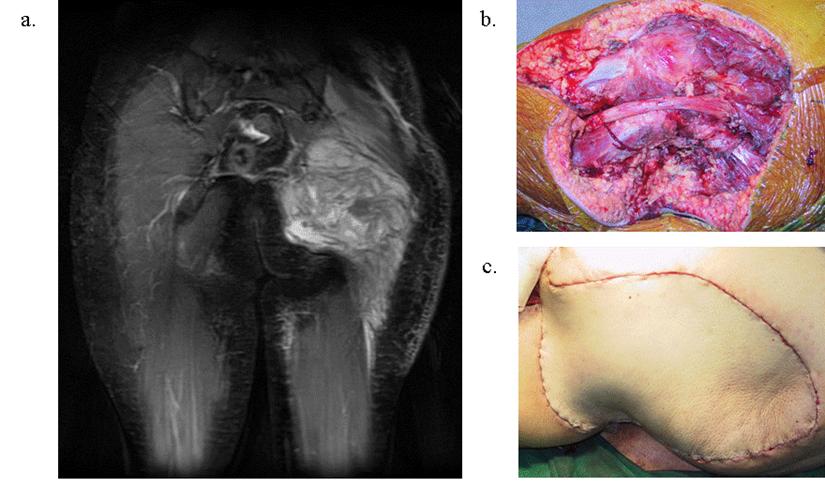
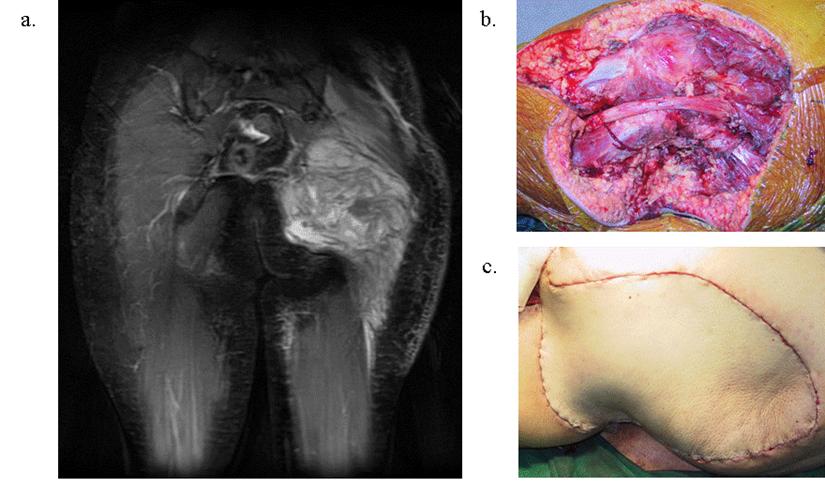
Our specialists have been trained to reconstruct these afflicted bones and joints so that patients with such conditions are able to lead their remaining lives out with dignity (Figure 3). Furthermore, our staff specifically ensures the great sensitivity needed towards such patients.
Benign tumours of the bones and soft tissues
These conditions are commonly encountered and treated by general orthopaedists and surgeons. Our special input in this field is in meeting two of the main challenges provided by these conditions.
Firstly, these conditions provide diagnostic problems - that is they can be mistaken for more serious conditions like cancers. Our service works closely with the Departments of Pathology and Radiology with whom we meet regularly and such cases are amply discussed before embarking on surgery. This minimises the risk of mis-diagnoses.
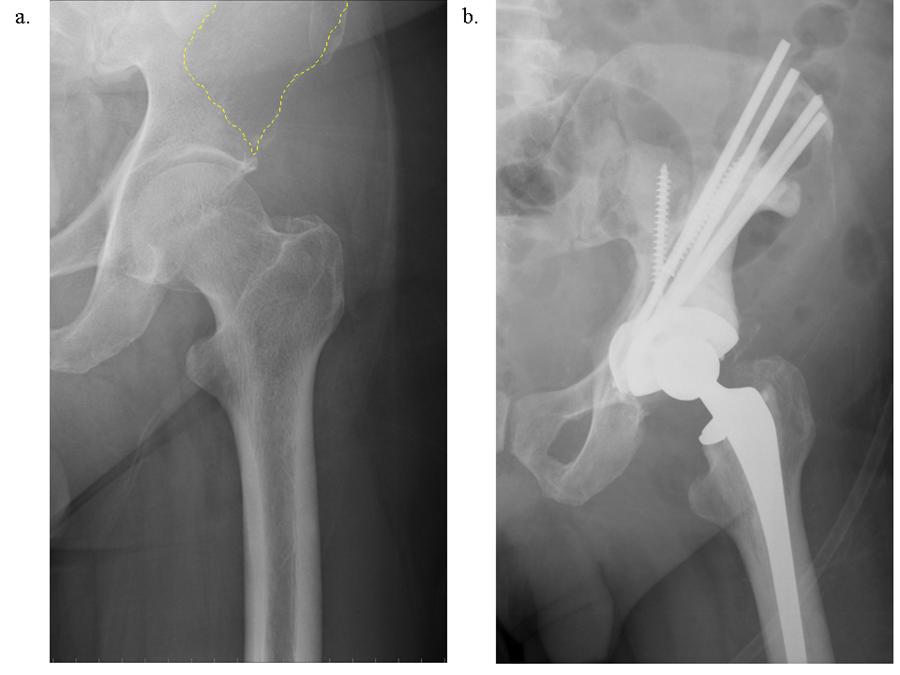
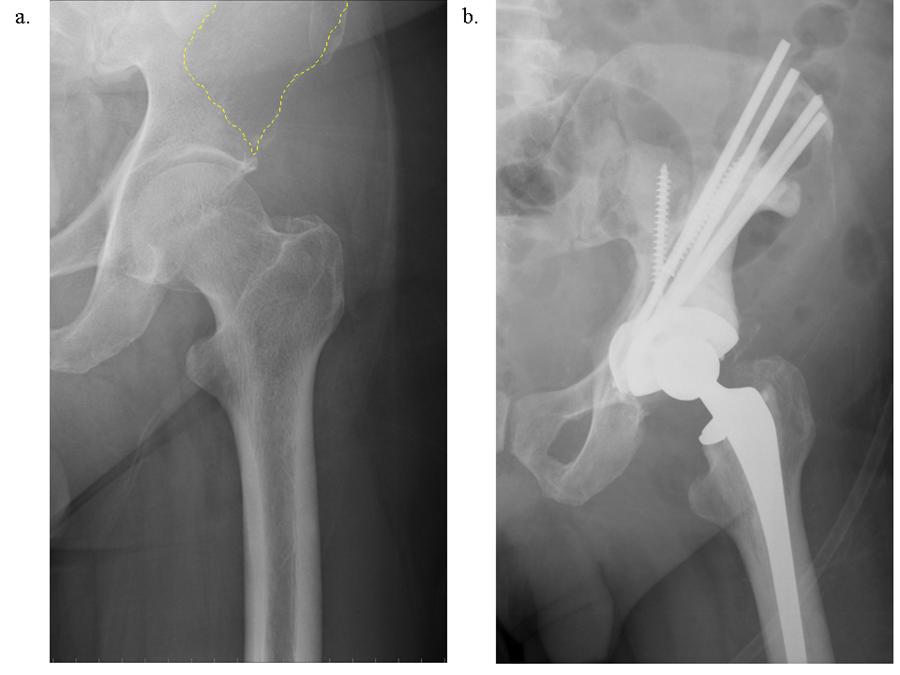
Next, when such conditions compromise function and need to be operated on (eg. Weakening the bone to the point that they may break) we would be able to reconstruct these conditions with minimal functional embarrassment (Figure 4).