- Pelvis—a basin-shaped structure, comprising the pubis in front and the sacrum and coccyx behind, that support the weight of the upper body and transmits weight-bearing to the lower extremities.
- Acetabulum—the cup-shaped cavity at the base of the pelvis into which the ball-shaped head of the femur fits (upper portion of the hip joint).
- Fragility Fractures—occur in osteoporotic bone, generally affecting elderly patients.
- Polytrauma—a short verbal equivalent used for patients usually with two or more severe injuries in at least two areas of the body.
- Non-union—failure of a fracture to unite.
- Mal-union—a bone which heals in a non-anatomic position (out of alignment).
- Limb Length Discrepancy—describing one limb being shorter than the other.
- Spine—the series of vertebrae forming the axis of the skeleton that protects the spinal cord.
Plevis and Acetabular Fractures
Fractures of the pelvis and acetabulum are among the most serious injuries treated by orthopaedic surgeons. These injuries usually result from high velocity accidents, such as in motor vehicles or high falls. People of all ages are vulnerable to these injuries. Elderly patients with fragile bones due to osteoporosis, in particular, can sustain fractures of the pelvis and acetabulum with a lower impact fall.

As with all fractures, we prioritise the patient's ability to return comfortably to normal daily activities. Acetabular fractures, injuring the joint bone and cartilage, occur through the socket of the hip joint. These fractures are often dislocated and require treatment to minimize the fracture. If joints heal with displaced bones, the surfaces will have irregularities, causing excessive wear and resulting in severe joint arthritis, reduced motion and function, along with pain. Proper alignment of the bones during healing is essential.
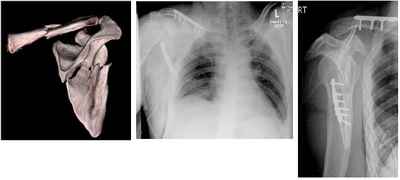
Stable pelvic fracture (no displacement or dislocation) may usually be treated without surgery. Displaced fractures usually require bone. This may be done by either open (surgical) or closed means (non-surgical). Once the bones are realigned with metallic devices including wires, pins, screws, and plates, the surgeon treats the bones internally or externally during healing.
Patients with pelvic fractures may require one or more surgical procedures. After reducing the fracture, the surgeon may use an External Fixation (Ex-Fix) frame to hole the bones in place. Application of an external fixator is done by inserting threated pins into the bone on either side of the fracture. These pins are then connected to rods outside the skin to form a frame.

While the Ex-Fix technique is sometimes the only procedure needed to repair a fractured pelvis, some patients require additional surgery in which plates and screws are used internally to hold the bones in place. Depending on the site and complexity of the fracture, the surgeon may have to fix the front or back of the pelvis, or both. Separate operations may be needed for each area needing treatment.
Patients with acetabular fractures often require Open Reduction with Internal Fixation (ORIF), especially those patients with joint displacement. The surgeon realigns the bones precisely to minimize the risk of developing post-injuring related problems, especially arthritis. Plates and screws prevent future displacement and facilitate early rehabilitation.
Treatment for acetabular fractures typically commences 5-10 days after the injury to mitigate the risk of intraoperative bleeding. During this period, patients may be placed in traction as part of an injury prevention program to avoid additional harm.
Complications
Throughout treatment and recovery, healthcare staff monitor for the following potential complications:
- Deep vein thrombosis and pulmonary embolism: Blood clots that may form in the veins of the pelvis, thigh and/ or lower legs and may travel to the lungs.
- Pneumonia: an infection of the lungs that may affect any bed-confined patients who cannot fully expand the lungs as per normal
- Skin problems resulting from being in one position for an extended period of time
- Muscle complications due to inactivity.
- Heterotopic ossification: an abnormal bone formation in an area where there is normally muscle; requiring prompt treatment to prevent this new bone from interfering with joint movement
- Damaged femoral head: If the joint's articular cartilage lining is affected in a pelvic injury, particularly in acetabulum fractures, the joint surfaces must be kept from rubbing together to reduce the risk of arthritis. Preoperatively, traction or a system of ropes, pulleys and weights are used to relieve pressure in the joint. Surgery with open reduction and internal fixation will securely realign the joints for immediate mobilzzation, preserving the smooth cartilage lining and preventing subsequent arthritis.
- Avascular necrosis of the femoral head: Patients with dislocated hips or acetabulum fractures, or both, may have disrupted blood flow to the femoral head (the ball in the hip joint). This can result in the death and collapse of bone tissue and hip joint arthritis.
- Nutritional problems: The body requires more protein and calories during healing.
- Constipation resulting from inactivity.
- Infection at the site of the injury.