Strabismus, commonly known as squint, is a prevalent condition among young children that may affect their sight, appearance and confidence if not detected and treated early. Every young child should have his eyes checked regularly. The treatment of squint is safe and effective, but its success requires the full cooperation of parents.
What Is A Strabismus/Squint?
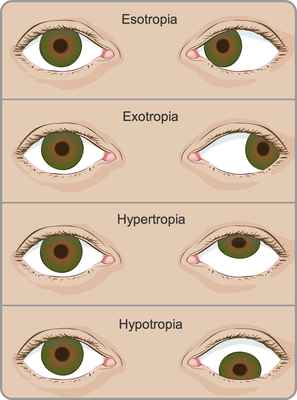
Strabismus is a condition that causes an individual’s eyes to point in different directions. In normal vision, both eyes are pointed straight at that object. If one eye points straight while the other eye turns away, it indicates strabismus.
How Does A Squint Affect My Child?
A squint can impact a child's vision, potentially leading to a condition known as a 'lazy eye', where the affected eye may not see clearly. Early detection and treatment are crucial for the effective cure of a 'lazy eye'. The timeliness of intervention significantly influences the outcome.
Individuals with a squint can only use one eye at a time, affecting their ability to judge distances and depth accurately. This, in turn, can affect the child's career and sports preferences in the future. Additionally, a squint can have implications for a child's appearance and self-confidence. Hence, there may be a preference for early surgical intervention to address the squint.
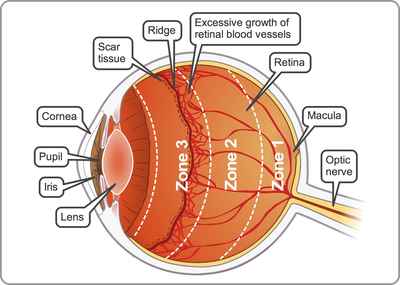
Finally, it is important to note that an eye with a squint may be associated with other underlying conditions that require appropriate treatment. Early assessment and intervention can play a pivotal role in addressing these associated conditions.
What Causes A Squint?
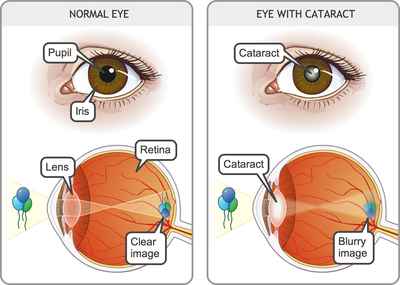
There are many causes. It may be due to a disorder of a part of the brain controlling eye movements or it may be caused by weak eye muscles, heredity, cataract, and nerve conditions. Also, any eye with poor sight tends to squint.
What Are The Treatment Options?
A child with a squint needs a full eye examination. This process may take time, especially as young children can be uncooperative and may require sedation..
Treatment strategies may include a combination of patching, spectacles, eye drops, eye exercises and in certain cases, surgery. The effectiveness of spectacles in correcting refractive errors depends on consistent wear, which can be a challenge with children. Parents play a crucial role in ensuring that their child wears spectacles regularly.
The treatment of a 'lazy eye' often involves patching the good eye to encourage the use of the 'lazy eye', enhancing the overall results of surgery. If patching or eyeglasses prove ineffective, surgery is recommended to straighten the eyes, improving both appearance and the ability to use both eyes together.
How Is A Squint Surgery Performed?
Squint surgery is an operation on the muscles that move the eye. Strabismus surgery involves tightening the weak muscles and/or loosening the stronger ones so that the eyes are positioned better. Special absorbable stitches will hold the eye muscles in their new position. The surgeon will not cut the skin around the eye, take the eye out of its socket, or use any lasers during the operation.
Sometimes both eyes need to be operated upon but this provides hardly any risk to the eye.
What Are The Risks Of Surgery?
It is considered a minor operation, with life-threatening or blinding complications being very rare. Children will receive general anaesthesia and be asleep throughout the surgery, which is very safe for healthy children. While double vision may occur after the operation, it usually resolves without treatment after a few months.
How Long Will My Child Take To Get Well?
Squint surgery is usually performed as a day surgery, with the child admitted in the morning and allowed to return home on the same day. Follow-up appointments are scheduled for the next day and within one week. There will be little or no pain after the operation and the eye is not patched, allowing the child to resume normal study and play after a few days. Swimming should be avoided for a month.
Does It Run In The Family?
Although most individuals with squints do not have affected relatives and exhibit normal intelligence, there is a sporadic familial occurrence. Therefore, it is advisable to monitor other children in the family if a relative has a squint.