Whether it manifests as a dull, lingering ache or a relentless, piercing throb, most of us are no strangers to the torment of a headache.
Issue 1 | June 2023

 Subscribe and ensure you don't miss the next issue!
Subscribe and ensure you don't miss the next issue!
Headaches rank among the most common health concerns that people experience and healthcare professionals confront. Though rarely life-threatening, headaches can nonetheless be a debilitating, occasionally disabling, condition for many.
However, not all headaches are created equal. They come in various forms and are triggered by a range of factors. This complexity, coupled with the prevalent reliance on over-the-counter (OTC) painkillers, can inadvertently exacerbate the problem, turning a once-manageable discomfort into a chronic condition.
As such, understanding the different types of headaches, their prevalence, and the factors that influence them - including the role of therapeutics - is critical to nip them in the bud.
Decoding headaches
Headaches are generally split into two camps: primary and secondary. Dr Jonathan Ong, senior consultant in the Division of Neurology, Department of Medicine at the National University Hospital (NUH), sheds some light on this common ailment.
"Headaches are a complex symphony of physiological interactions, with nerves affecting muscles and blood vessels, which then signal the brain to register the discomfort," says Dr Ong.
Primary headaches include the infamous migraines, tension-type headaches that often resemble a tight band encircling your head, and the lesser-known cluster headaches. These are not symptoms of another medical illness but usually arise due to a dysfunction or overactivity of pain-sensitive structures in the head.
On the other side of the coin are secondary headaches, stemming from underlying medical conditions such as head injuries, strokes, infections, and disorders of the neck, eyes, nose, sinuses, or teeth. These headaches generally originate from structural disturbances or irritations - including stretching, dilatation, constriction, or stimulation of blood vessels, meninges, muscles, and cranial or spinal nerves - causing discomfort and pain.
When headaches strike, many tend to seek solace in OTC painkillers. Yet, here's a surprising caveat: the age-old saying, "too much of anything is bad for you", rings true when it comes to headache medication too.
"The tricky thing about the frequent usage of these drugs over a period of, say, three months, is that they can lose their effectiveness as your body gets used to them. This could potentially worsen the headache rather than resolve it," cautions Dr Ong, underscoring the double-edged nature of OTC therapeutics in headache management.
There's a potential risk for those who consume paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) for over half a month. Taking migraine medication or opioids (such as codeine-based medicines), as well as combination painkillers on 10 or more days a month can produce the same effect too.
A common yet disabling affliction
A 2022 study revealed that over half of the world's population experienced some type of primary headache in the preceding year. About one in seven individuals suffers from a headache daily.
Singapore mirrors this statistic, and according to Dr Ong, NUH's Neuroscience Clinic has reported a slight increase in patients diagnosed with headaches, particularly migraines, over the past year.
Migraines often manifest as more than an intense, pulsating pain in the head. They can make a person unusually sensitive to light and noise, and even bring on nausea or bouts of vomiting.
But the ramifications of migraines stretch beyond physical discomfort. They significantly impact societal and economic sectors as well. A 2019 study led by Dr Ong estimated that in 2018 alone, migraines cost Singapore a staggering S$1.04 billion.
A large portion of this sum - around 80 per cent - was due to productivity loss. The remaining 20 per cent was spent on healthcare services associated with managing migraines.
The study also unveiled that on average, respondents missed almost 10 workdays annually due to migraines. For those who managed to go to work, their productivity was severely affected.
When to seek medical help
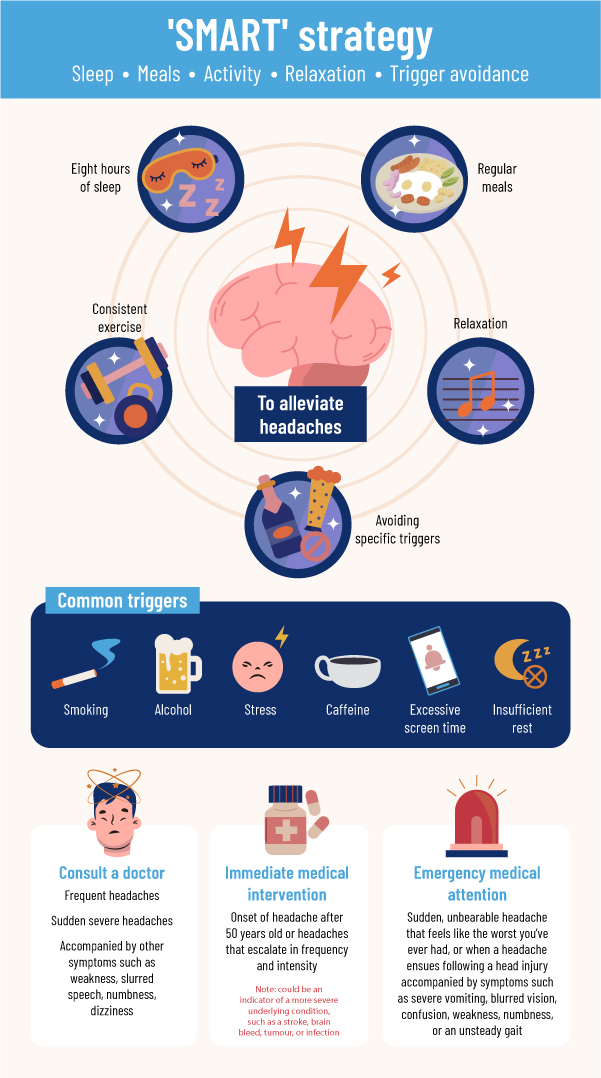
So how do we combat these pesky headaches? While they can be distressing, not every headache warrants a trip to the doctor's office. Most can be managed with a little self-care and lifestyle tweaks, as recommended by many other physicians.
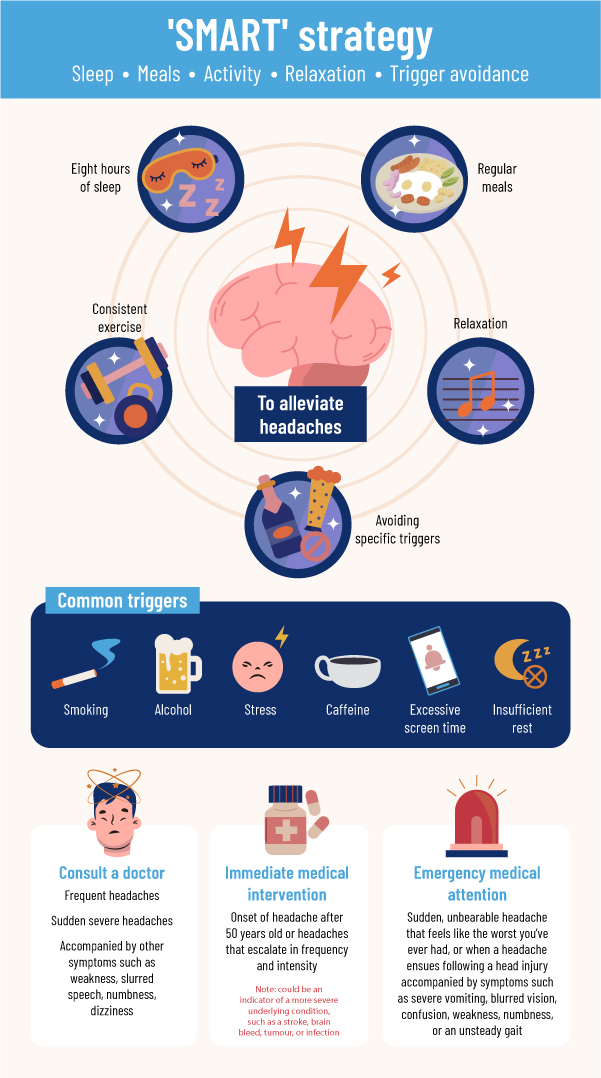
There's no one-size-fits-all solution for headaches. It's about striking a balance: treating the pain while avoiding potential issues from the over-reliance on medication. This management strategy involves a mix of medical advice, lifestyle modifications, and careful monitoring of OTC medication use.
With proper understanding and management, tackling headaches via a 'headache-free' approach is entirely feasible!
Like this article? Simply subscribe to make sure you don't miss the next issue of EnvisioningHealth!