A transplant team at NUH has given young Elvia Lim
a new chance at life with a liver transplant to manage
maple syrup urine disease, a rare metabolic disorder.
Issue 7 | December 2024

 Subscribe and ensure you don't miss the next issue!
Subscribe and ensure you don't miss the next issue!
At just 14 days old, Elvia was diagnosed with a sweet-sounding but potentially deadly condition — maple syrup urine disease (MSUD). Managing this rare metabolic disorder ensued strict dietary requirements and frequent check-ups to avoid life-threatening complications. Despite careful monitoring, Elvia’s health remained on the line.
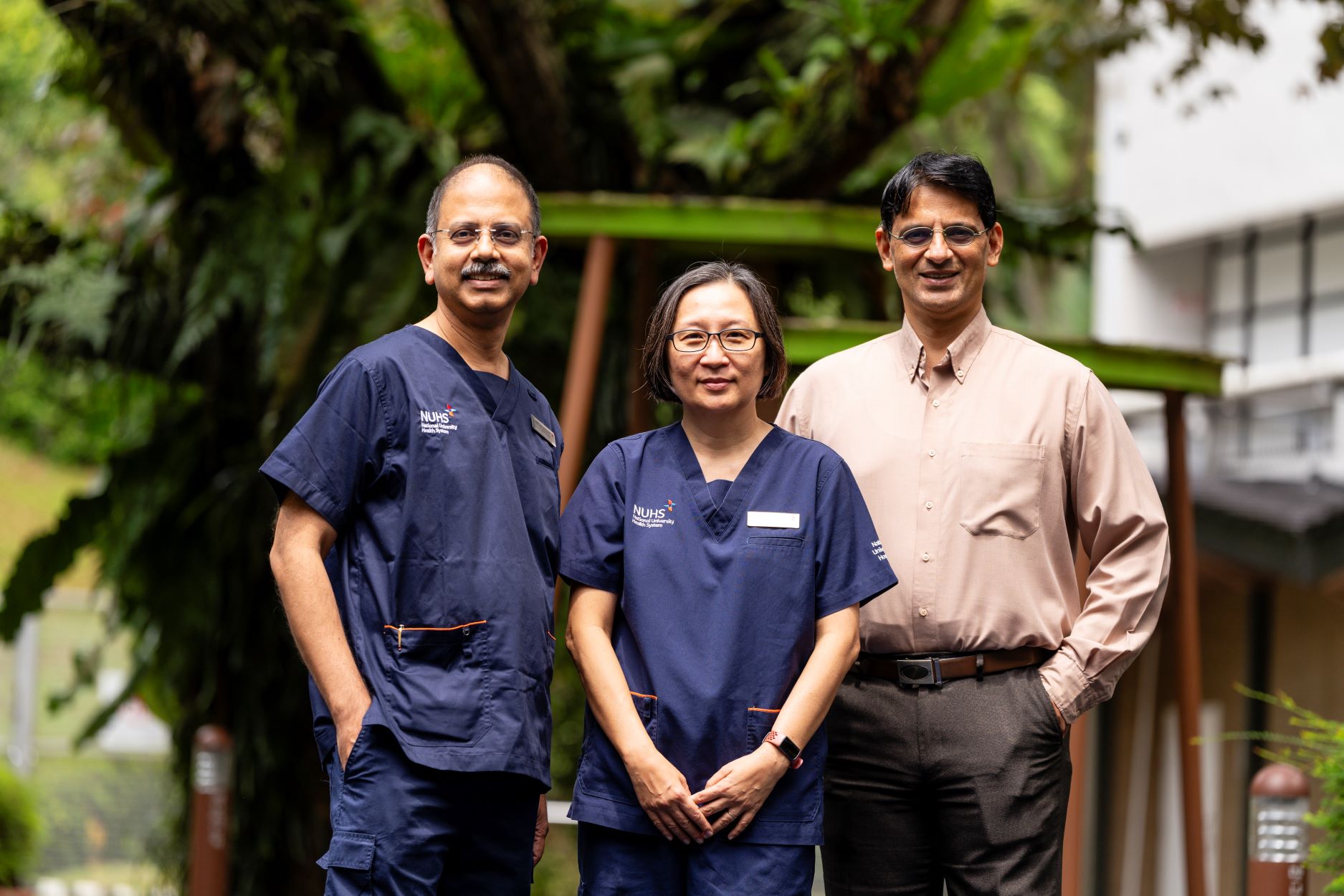
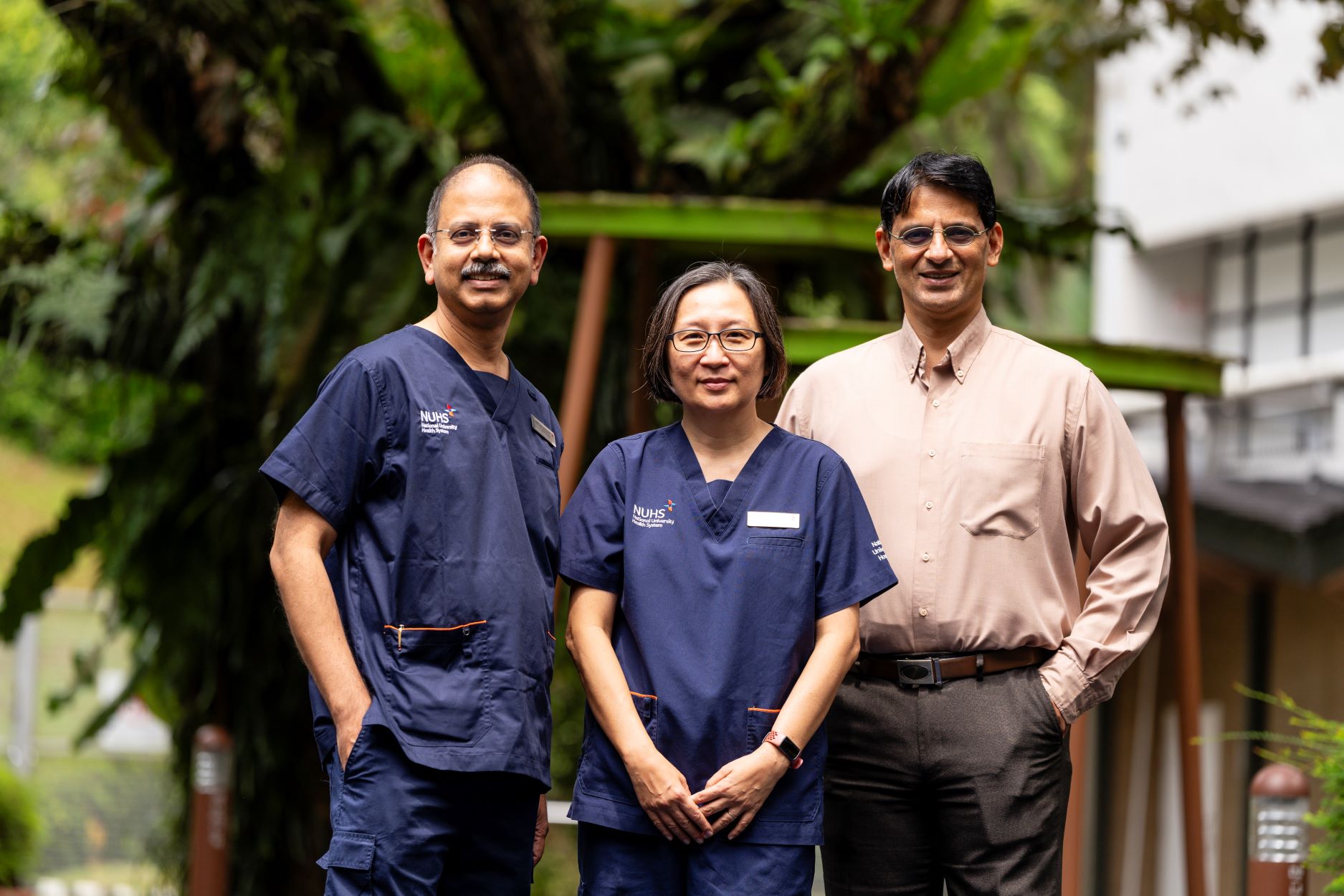
In 2021, her parents brought her to the National University Hospital (NUH) for a second opinion. By 2022, the medical team at NUH, led by Adjunct Associate Professor Vidyadhar Mali, Senior Consultant, Department of Paediatric Surgery, Khoo Teck Puat – National University Children’s Medical Institute (KTP-NUCMI)1, NUH, determined that a liver transplant was her best hope for a healthier future.
Dealing with a complex condition with the best care
MSUD is an inherited metabolic disorder in which enzymes responsible for breaking down certain amino acids fail to function properly. Without treatment, the resulting buildup of amino acids, especially leucine, in the blood can cause brain swelling, seizures and intellectual disabilities. In severe cases, infants may not survive beyond the first few weeks of life.
“MSUD affects an estimated one in 180,000 babies born. In Singapore, we expect one child in every five to six years to have this condition, and, as far as I know, we already had three in the last 18 years,” says Associate Professor Denise Goh, Head & Senior Consultant, Division of Genetics and Metabolism, Department of Paediatrics, KTP-NUCMI1, NUH, who was part of the team that took care of Elvia before and after her transplant.
For children like Elvia, managing MSUD requires round-the-clock vigilance and a strict low-protein diet to avoid dangerous amino acid spikes. But after multiple hospital visits and a diagnosis of laryngomalacia, Elvia’s parents learnt about the promising results liver transplantation could have for MSUD and decided to pursue this option to give their daughter a fighting chance at life.
In 2022, at age three, Elvia received a third of a donor’s liver in a 10-hour operation led by Adj A/Prof Mali, who is also the Surgical Director & Senior Consultant for the Paediatric Kidney and Liver Transplantation Programmes at the National University Centre for Organ Transplantation, NUH.
“Liver transplantation is an effective treatment and cure for MSUD. The donors selected do not have MSUD. Therefore, the donor liver contains the enzyme which is absent in MSUD patients. Following liver transplantation, these children can go on an unrestricted, normal diet without any risk of toxicity or brain damage. With more than 150 paediatric liver transplants performed over three decades, NUCOT Paediatric Transplant has the cumulative surgical expertise and experience for the smooth conduct of complex liver transplants such as Elvia’s. It was crucial to ensure a smooth operation for the liver to work immediately to prevent MSUD crisis during and after the transplant operation,” explains Adj A/Prof Mali.
Following the transplant, Elvia’s nutrition was managed by Dr S. Venkatesh Karthik, Senior Consultant, Division of Paediatric Gastroenterology, Nutrition, Hepatology and Liver Transplantation, Department of Paediatrics, KTP-NUCMI1, NUH. Dr Karthik will keep a watchful eye on her health until she turns 21, including overseeing her immunosuppressive medication to prevent organ rejection.
“After transplantation, children like Elvia will need to avoid raw foods and probiotics and practise careful hygiene,” adds Dr Karthik.
Today, Elvia is a thriving five-year-old. She attends pre-school, plays with her classmates and — aside from avoiding probiotic foods — eats like any other voracious child.
Building awareness for your child’s health
For parents facing similar challenges, early diagnosis and a well-informed, proactive approach can make a significant difference. In Elvia’s case, her parents’ commitment to learning about potential treatments — including liver transplantation — opened up options that transformed her quality of life.
“Beyond medical treatment, a strong support system is crucial. Families dealing with rare conditions often face emotional and logistical hurdles. Connecting with other parents, advocacy groups or counselling resources can make a meaningful difference. These networks offer both practical advice and emotional support, empowering families to make informed choices while managing the uncertainties that come with rare conditions,” advises A/Prof Goh.
1KTP-NUCMI is part of the National University Centre for Women and Children (NUWoC), a national university specialist centre that aims to empower women, children and their families to lead healthier lives.
Like this article? Simply subscribe to make sure you don't miss the next issue of EnvisioningHealth!