- Dementia
- Delirium
- Falls
- Functional Decline
- Dementia
What is dementia?
Dementia is a general term describing a group of symptoms that are often progressive, including:
- Memory loss
- Mood changes
- Communication difficulties
- Reasoning problems
- Challenges in completing day-to-day tasks
These symptoms may occur individually or in combination. Initially, memory loss and cognitive difficulties can be troubling for the senior with dementia. They may become apathetic or lose interest in usual activities, face challenges in social situations and show emotional control issues. Some individuals may develop agitation, disruptive behaviour and hallucinations.
Often, seniors with dementia may not be aware of these issues as they gradually lose the ability to remember events or fully comprehend their environment.
How does dementia progress?
Dementia is progressive, meaning symptoms worsen over time. In advanced stages, individuals may become highly dependent and lose significant communication abilities. The progression rate varies between individuals and depends on the type of dementia.
What causes dementia?
Dementia can result from various conditions, including:
The most common form, accounting for 60– 80% of cases. It is caused by changes in brain chemistry and structure, leading to cell death. Short-term memory issues are often the first sign.
Vascular dementia
Arises from inadequate blood and oxygen supply to the brain, leading to cell death. It can occur post-stroke or due to damaged brain arteries.
Dementia with Lewy bodies (DLB)
Named after the abnormal structures, Lewy bodies, that build up in brain nerve cells. It affects brain tissue function, causing symptoms like falls, confusion, hallucinations, reasoning difficulties and memory impairment. DLB shares similar characteristics with Parkinson's disease dementia but with a different trajectory.
Fronto-temporal dementia
Often affects younger individuals and results from damage to the brain's frontal part, leading to personality and behavior changes.
Mixed dementia
Common in advanced age (85+), it's often a combination of Alzheimer’s disease and vascular damage.
Other causes of dementia
Includes cumulative brain damage from chronic alcoholism or repeated head injuries (e.g. former professional boxers or football players).
Back to Top
What is mild cognitive impairment?
MCI involves memory problems but not severe enough for dementia diagnosis. Individuals with MCI are at a higher risk of developing dementia, but it's not a certainty.
What is the difference between dementia and delirium?
Both cause memory loss and confusion, but delirium is usually reversible and has an acute onset.
Why is it important to get a diagnosis?
Early diagnosis of dementia allows for interventions to slow its progression and preserve memory. It helps seniors get appropriate treatment and support and assists their families in planning for the future. Many seniors can lead active and fulfilled lives with proper treatment and support.
How is dementia diagnosed?
Diagnosis can be made by a GP or a specialist (geriatrician, neurologist or psychiatrist). It may involve cognitive tests, blood tests, brain scans or more in-depth memory and cognitive skills assessments.
Can dementia be cured?
Most dementia types are incurable, but research continues on potential treatments. Delaying or preventing dementia onset may be possible through lifestyle changes (education, managing hearing loss, addressing hypertension, reducing obesity, quitting smoking, treating depression, increasing physical activity, controlling diabetes and socialisation).
Some drugs can temporarily alleviate symptoms including cholinesterase inhibitors (Donepezil, Rivastigmine and Galantamine) and Memantine.
These medications should be periodically evaluated for effectiveness. While they don’t cure Alzheimer’s, early treatment can potentially improve life quality for a longer period.
Delirium
What is delirium?
Delirium is a medical condition characterized by sudden confusion. Individuals with delirium may struggle with attention, recognition of their surroundings and memory. Symptoms can vary throughout the day and often intensify in the evenings.
If you suspect a loved one is experiencing delirium, prompt evaluation by a doctor is vital to identify and treat the underlying causes. Alert your healthcare provider immediately.
What causes delirium?
Delirium in seniors can be triggered by various factors, including:
- Infections (senior may not always exhibit a fever but rather a change in mental status)
- Medications, especially those with a high anticholinergic load
- Pain
- Dehydration
- Constipation
Certain factors can predispose seniors to delirium:
- Environmental changes, such as hospitalisation
- Use of multiple medications
- Existing underlying dementia
- Poor eyesight or hearing
How common is delirium?
Delirium is relatively common among seniors, occurring in up to one-third of those admitted to hospitals. It is more prevalent in intensive care units or during the perioperative period.
How do we treat delirium?
Treatment for delirium involves:
- Addressing the underlying cause. Alongside acute treatment, we support patients by maintaining a calm environment, orienting them to their surroundings and explaining the reason for their hospital stay
- Alleviating pain and minimising discomfort
- Encouraging a regular sleep-wake cycle when possible
- Making hearing aids and eyeglasses available if the patient uses them at home
- Removing barriers and restraints, including urinary catheters, where possible
- Promoting mobility and cognitive activities
Family presence can be beneficial for patients with delirium. Familiar faces and support from loved ones can be comforting and helpful during their hospital stay.
Falls are common incidents, particularly in older individuals or those with long-term health conditions. While many falls do not result in serious injury, they can sometimes lead to significant harm, such as broken bones and can affect a person's confidence and independence.
What causes a fall?
The risk of falling increases with age due to factors like:
- Balance problems and muscle weakness
- Poor vision
- Impaired sensation or foot pain
- Long-term health conditions, such as heart disease, dementia or low blood pressure
- Vitamin D deficiency
- Medications affecting attention (e.g. opioid analgesics, antianxiety drugs, and some anti-depressant drugs) or lowering blood pressure (e.g. antihypertensive, diuretic, and some heart drugs), including some over-the-counter medicines
- Poor safety awareness
Falls can also be caused by physical conditions that impair mobility or balance, hazards in the environment, or potentially hazardous situations. A fall is also more likely to happen when:
- the floor is wet or has been recently polished, such as in the bathroom
- the lighting in the room is dim
- rugs or carpets aren't properly secured
- the person is reaching for storage areas, such as a cupboard, or is going down stairs
- the person is rushing to get to the toilet
- there are electrical or extension cords or objects that are in the way of walking
- there are uneven sidewalks and broken curbs
- the person is unfamiliar with his/her surroundings
Most falls occur when several causes interact. For example, people with Parkinson’s disease and impaired vision (physical conditions) may trip on an extension cord (an environmental hazard) while rushing to answer the telephone (a potentially hazardous situation). The more risk factors a person has, the greater their chances of falling.
What are the symptoms and consequences of a fall?
Falls often occur without warning, but physical conditions can sometimes cause pre-fall symptoms like dizziness, light-headedness or heart palpitations. Injuries from falls, such as bruises, sprains, or broken bones, can be more severe with age. Falls can also lead to a fear of falling, reducing activity levels and increasing the risk of future falls.
What can happen after a fall?
Falls can cause broken bones, like wrist, arm, ankle, and hip fractures. These injuries can make it hard for a person to get around, do everyday activities, or live on their own.
Falls can cause head injuries. These can be very serious, especially if the person is taking certain medicines (e.g. blood thinners). An older person who falls and hits his/her head should see a doctor right away to make sure they don’t have a brain injury.
Some falls can be serious and result in death.
The effects of a fall may last a long time. Many people who fall, even if they’re not injured, become afraid of falling. This fear may cause a person to cut down on their everyday activities. When a person is less active, they become weaker and this increases their chances of falling.
Should I tell my doctor if I have fallen?
It is vitally important for people to tell their doctor if they have fallen, even if the doctor has not asked, so that the doctor can uncover treatable reasons behind the fall. People who have fallen may be reluctant to tell their doctor because they think falling is just part of getting older, especially if they have not been injured. Even people who have been seriously injured during a fall and have been treated in an emergency department may be reluctant to admit they have fallen.
Some older people may be reluctant to seek help and advice from their GP and other support services about preventing falls, because they believe their concerns won't be taken seriously. However, all healthcare professionals take falls in older people very seriously because of the significant impact they can have on a person's health.
How are falls treated?
Initial treatment focuses on injuries, such as head injuries, fractures, sprained ligaments and strained muscles.
Subsequently, addressing underlying disorders and improving walking and balance through physical and occupational therapy is essential. These therapies also build confidence and suggest preventive measures.
How can you prevent falls?
To reduce the risk of falls:
- Discuss fall risks and medication reviews with your doctor.
- Engage in strength and balance exercises.
- Ensure appropriate clothing and footwear.
- Regularly check your eyesight and update eyeglasses.
- Make your home safer with grab bars, non-slip mats, good lighting and removing tripping hazards.
- Limit alcohol consumption to avoid coordination and balance issues.
Talk to your doctor to
- evaluate your risk for falling and talk with them about specific things you can do
- review your medicines to see if any might make you dizzy or sleepy. This should include prescription medicines and over-the-counter medicines. Your doctor may recommend alternative medication or lower doses if they feel the side effects increase your chances of having a fall. In some cases, it may be possible for the medication to be stopped.
- Do strength and balance exercises
- Do exercises that make your legs stronger and improve your balance. This can take the form of simple activities such as walking and dancing, or training programmes. Tai Chi is a good example of such an exercise.
- Have proper clothes and footwear
- Avoid loose-fitting, trailing clothes that might trip you
- Wear well-fitting shoes that are in good condition and support the ankle
- Take care of your feet by trimming your toenails regularly and seeing a doctor about any foot problems
Have your eyes checked
Have your eyes checked by an eye doctor at least once a year, and be sure to update your eyeglasses if needed. If you have bifocal or progressive lenses, you may want to get a pair of glasses with only your distance prescription for outdoor activities, such as walking. Sometimes these types of lenses can make things seem closer or farther away than they really are. Not all visual problems can be treated. However, some problems, such as cataracts, can be surgically removed with surgery.
Make your home safer
- Add grab bars inside and outside your bathroom
- Use non-slip mats in the bathroom
- Mop up spills to prevent wet, slippery floors
- Get help lifting or moving items that are heavy or difficult to lift
- Remove clutter that you could trip over
- Ensure all areas of the home are well lit
- Avoid alcohol
Drinking alcohol can lead to loss of co-ordination and exaggerate the effects of some medicines. This can significantly increase the risk of falls, particularly in older people. Avoiding alcohol or reducing the amount you drink can reduce your fall risk. Excessive drinking can also contribute to the development of osteoporosis.
If you've fallen in the past, making changes to reduce your chances of falling can also help you overcome any fear of falling.
What should you do if you fall?
If uninjured, get up slowly using stable furniture for support. If injured or unable to get up, attract attention for help, and if possible, reach for a phone to call for assistance. Keep a telephone accessible from the floor or consider a personal emergency response system.
Functional Decline
What is Functional Decline?
Ageing impacts all aspects of our bodies and lives. While living longer is desirable, living well is equally important. Maintaining independence is an important aspect of a high-quality life, making the preservation of function in elderly individuals a top priority.
Function: the ability to take care of him/herself. This includes having the physical strength to do things as well as the mental ability to plan these actions.
Decline:this means the older person is not able to do what he/she was able to do before. This varies from person to person.
Functional decline can manifest in various forms, with common signs including:
- Reduced appetite
- Increased sleepiness, loss of interest and withdrawal
- Decreased communication with family
- Reduced mobility
- Urinary incontinence
What causes Functional Decline?
Functional decline can be triggered by many factors, such as:
- Medical conditions such as infections, strokes or heart attacks.
- Reduced food and fluid intake, leading to decreased energy.
- Feelings of sadness or withdrawal, reducing motivation.
- Delirium due to environmental changes or infections.
- Impaired vision or hearing.
- Lack of sleep.
- Changes in social circumstances, such as new housing or caregivers
What does it mean for my loved ones?
Functional decline can create a cyclical pattern where causes and effects perpetuate each other (see diagram below). This highlights the importance of early identification, treatment and prevention.

Effects of functional decline
What can loved ones do?
Support is crucial for family members experiencing functional decline. It’s important not to attribute these changes solely to ageing. Seeking a consultation with a geriatrician or physician specialising in geriatric care is advisable. The presence and support of loved ones can be incredibly comforting and motivating for older adults. A CGA conducted by geriatricians and a trained team can help identify the causes of functional decline, focus on the patient's strengths and find solutions to enhance their quality of life. Treatment may involve addressing acute medical conditions, improving function, memory, environment and/or mood.


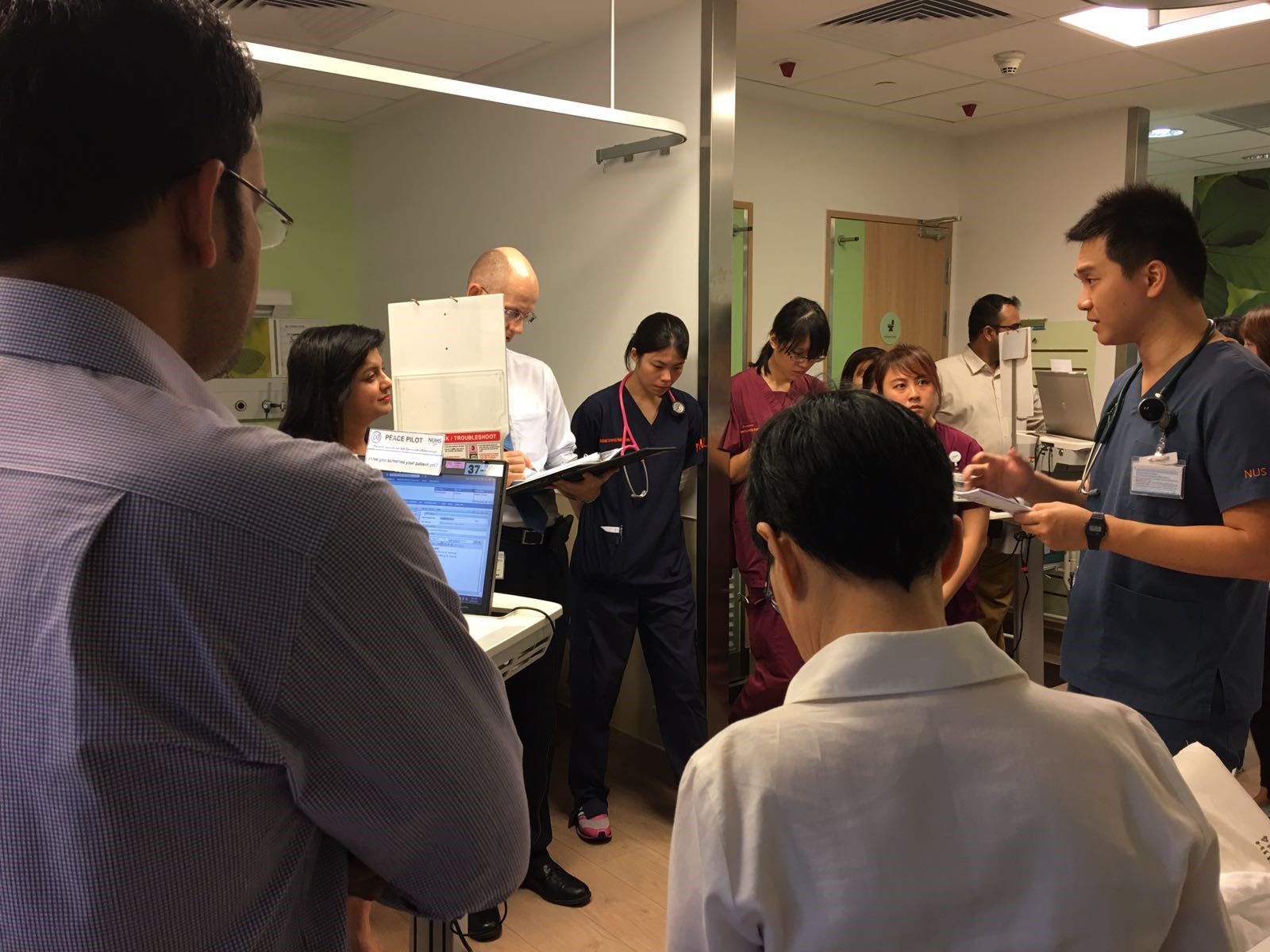
 Nurses Improving Care for Healthsystem Elders (NICHE) is an international quality and safety program that enhances clinical nursing in the care of older adults. NICHE provides principles, tools, education and resources to empower healthcare organizations to improve health outcomes for older adults by addressing their unique needs and implementing evidence-based practices. NUH has been a member of NICHE since 2016 and we are dedicated to improving the quality of care older adults receive. Foundation to NICHE is the Geriatric Resource Nurse Model in which Registered Nurses are trained to become unit-based resource persons with regards to geriatric nursing care issues, geriatric care standards and practices. Through this programme, we have groomed and equipped Geriatric Resource Nurses (GRNs) with knowledge and skills in these vital areas, with the aim of improving patient outcomes and experiences. GRNs are now present in most adult wards, where they can perform Comprehensive Geriatric Assessments and provide advice on nursing care management for older patients with complex issues. Geriatric care nursing standards are enhanced through GRN’s leadership roles and acting as agents of change within their wards. Our commitment to improving the quality of care for older adults is not just a mission statement; it is the very foundation upon which we operate. This unwavering dedication and exceptional care have been recognized and awarded the Exemplar Recognition Status by NICHE in October 2025. This recognition signifies that our hospital has not only met but exceeded the rigorous standards set by NICHE, demonstrating our ongoing pursuit of excellence in geriatric care practices.
Nurses Improving Care for Healthsystem Elders (NICHE) is an international quality and safety program that enhances clinical nursing in the care of older adults. NICHE provides principles, tools, education and resources to empower healthcare organizations to improve health outcomes for older adults by addressing their unique needs and implementing evidence-based practices. NUH has been a member of NICHE since 2016 and we are dedicated to improving the quality of care older adults receive. Foundation to NICHE is the Geriatric Resource Nurse Model in which Registered Nurses are trained to become unit-based resource persons with regards to geriatric nursing care issues, geriatric care standards and practices. Through this programme, we have groomed and equipped Geriatric Resource Nurses (GRNs) with knowledge and skills in these vital areas, with the aim of improving patient outcomes and experiences. GRNs are now present in most adult wards, where they can perform Comprehensive Geriatric Assessments and provide advice on nursing care management for older patients with complex issues. Geriatric care nursing standards are enhanced through GRN’s leadership roles and acting as agents of change within their wards. Our commitment to improving the quality of care for older adults is not just a mission statement; it is the very foundation upon which we operate. This unwavering dedication and exceptional care have been recognized and awarded the Exemplar Recognition Status by NICHE in October 2025. This recognition signifies that our hospital has not only met but exceeded the rigorous standards set by NICHE, demonstrating our ongoing pursuit of excellence in geriatric care practices.