Artificial intelligence and mixed reality are transforming healthcare at NUH, redefining many procedures from CT scans to patient consultations—bringing enhanced outcomes previously unattainable.
Issue 1 | June 2023
 Subscribe and ensure you don't miss the next issue!
Subscribe and ensure you don't miss the next issue!
Advancements in technology have the power to reshape industries, and healthcare is no exception.
From the lab to bedside, artificial intelligence (AI) and mixed reality (MR) are not just sparking revolutions - they are recalibrating the way medicine is practised, charting new frontiers at the intersection of healthcare and technology.
Rapid decision-making, rapid recovery
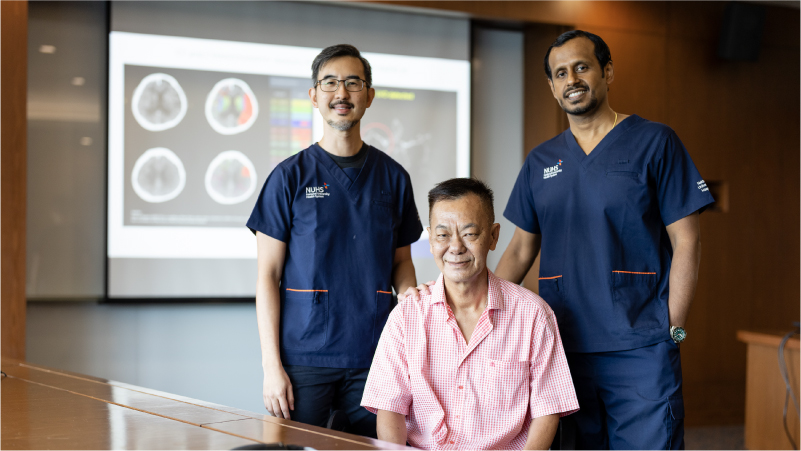
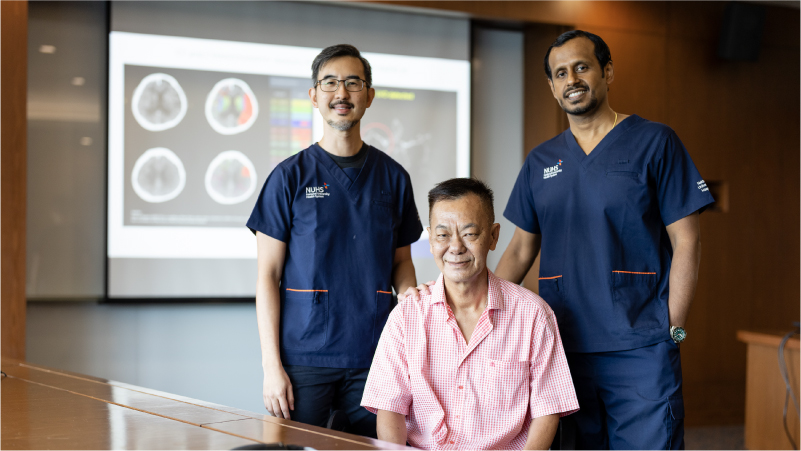
Leading the way in this transformation is the National University Hospital (NUH), the tertiary hospital of the National University Health System (NUHS). NUH is at the forefront of deploying RapidAI, an AI-based neuroimaging software, to expedite the identification of stroke patients who could potentially benefit from endovascular treatment.
RapidAI can process large volumes of raw data from computerised tomography (CT) scans in less than a minute to generate easy to interpret images providing objective information — a vast improvement over the traditional 20-minute manual processing. Besides post processing, it also facilitates instantaneous dispersal of this vital information to all the stake holders (senior physicians who make the therapeutic decisions), directly into their secured email inboxes. This improvement in workflow has already benefitted over 400 patients, dramatically enhancing the efficiency of their treatment.
"The benefits of this AI-powered technology extends beyond sheer speed. It provides the medical team with vital, colour-coded images, supplemented with quantitative data, that shed light on the extent of brain damage a patient has sustained and the volume of brain at risk," said Adjunct Associate Professor Anil Gopinathan, Head and Senior Consultant, Division of Interventional Radiology, Department of Diagnostic Imaging at NUH.
RapidAI not only identifies but also quantifies the potential gains of mechanical thrombectomy, a procedure to remove blood clots blocking the arteries of the brain. By presenting the interventional radiologists and stroke neurologists with comprehensive and quantitative imaging data, RapidAI empowers them to make swift, data-driven decisions. By reducing the delay in unblocking the arteries of the brain, it helps in reducing brain damage and long term disability.
"When you consider that each passing minute can result in the loss of millions of brain cells, the accelerated processing of RapidAI offers us a critical advantage. It's akin to a sprinter's explosive start - an edge that can ultimately determine the race's outcome. And in our case, it improves the likelihood of a stroke patient walking out of the hospital," explains Adj A/Prof Gopinathan.
Bringing mixed reality to life
Parallel to AI's breakthroughs, MR is making headway at NUHS this year. One notable innovation is the application of 5G-enabled ultrasound scans, which drastically curtail patients' wait times.
In the near future, doctors donning MR visors, can view these scans in real-time, facilitating rapid and accurate diagnoses. This innovation is especially useful for routine thyroid cancer checks—traditionally a weeks-long scheduling affair.
"With MR, we're not only speeding up routine checks, but are also freeing up resources for more urgent scans while easing patients' anxiety, as quicker results mean less uncertainty," says Dr Gao Yujia, a consultant in the Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery at NUH. He is also Assistant Group Chief Technology Officer at NUHS.
But the impact of MR extends beyond diagnostics — it also promises to revolutionise surgical procedures and patient consultations. In the operating theatre, surgeons wear MR headsets to view 3D renderings of a patient's anatomy, similar to having a digital blueprint for guidance.
Meanwhile, in consultation rooms, both doctors and patients wear headsets to review surgical procedures. Using 3D models, they can visualise operations and better understand potential risks. "This provides more insight for patients and helps us create a common understanding — it's about combining empathy with precision," adds Dr Gao.
The blend of AI and MR offers a tantalising glimpse into the future of healthcare—a future where advanced technologies aren't just adjunct, but integral parts of healing, augmenting human capabilities and setting new standards in modern healthcare.
Like this article? Simply subscribe to make sure you don't miss the next issue of EnvisioningHealth!