Nerve stimulation, also known as neuromodulation, is a treatment option for overactive bladder when medications prove ineffective or when intolerable side effects arise. It is also considered for individuals experiencing urinary symptoms caused by neurological conditions.
Nerve stimulation involves the application of electrical pulses to stimulate the sacral nerves responsible for controlling the bladder and the urination cycle.
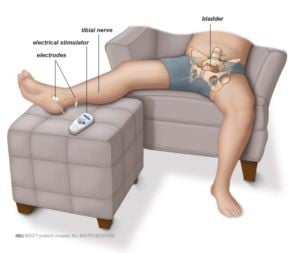
PTNS uses a needle at the level of the ankle to stimulate the tibial nerves which, in turn, affects the sacral nerves.
Tibial nerve stimulation During this procedure, a thin needle connected to an electric current is placed near the ankle. The needle penetrates the skin, stimulating the tibial nerve which extends from the inner part of the ankle, along the leg, up to the sacral nerves in the lower back (Fig. 1).
A treatment course for tibial nerve stimulation generally
includes 12 sessions, conducted weekly at the clinic, each lasting 20-30 minutes. As the initial effects may wear off over time, additional treatment courses may be needed after the initial 12 sessions.
PTNS is generally well-tolerated with minimal side effects. Mild pain may be experienced when the needle is being placed, but this subsides once the needle is removed. During the procedure, some individuals may feel a slight aching sensation when the current is running through.