Services for Prostate Cancer
2024/05/15
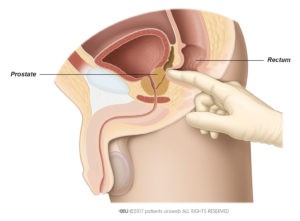
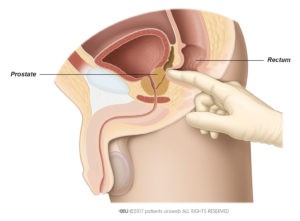
A prostate check, or digital rectal examination, is a quick and simple test to assess the possibility of a prostate problem. During this examination, the doctor will insert a gloved and lubricated finger into the rectum to palpate the prostate.
Prostate-specific antigen (PSA) is a protein produced only by the prostate. High PSA levels can result from many reasons, including infection, benign prostatic growth and prostate cancer. If the PSA levels are elevated, further tests will be recommended to rule out a diagnosis of prostate cancer.
What happens if my PSA level is high or my prostate is abnormal on a rectal examination?
Your doctor will discuss available tests with you and use the results assess your risk of having prostate cancer. At NUH, the screening options include the prostatic health index (PHI), prostate MRI and a trans-perineal biopsy of the prostate gland.
The Prostate Health Index (PHI) test is a diagnostic blood test that calculates a personalised risk of underlying prostate cancer. It aims to minimise unnecessary prostate biopsies and assist patients in making informed decisions regarding further investigations.
Magnetic resonance imaging, or MRI scan, generates detailed images of the internal structures of your body using magnets and radio waves. It offers provides a thorough examination of the prostate, aiding the doctor in determining the necessity of a biopsy. Moreover, MRI images can be used to enable targeted biopsies of suspicious areas, thereby increasing the accuracy of prostate biopsies.
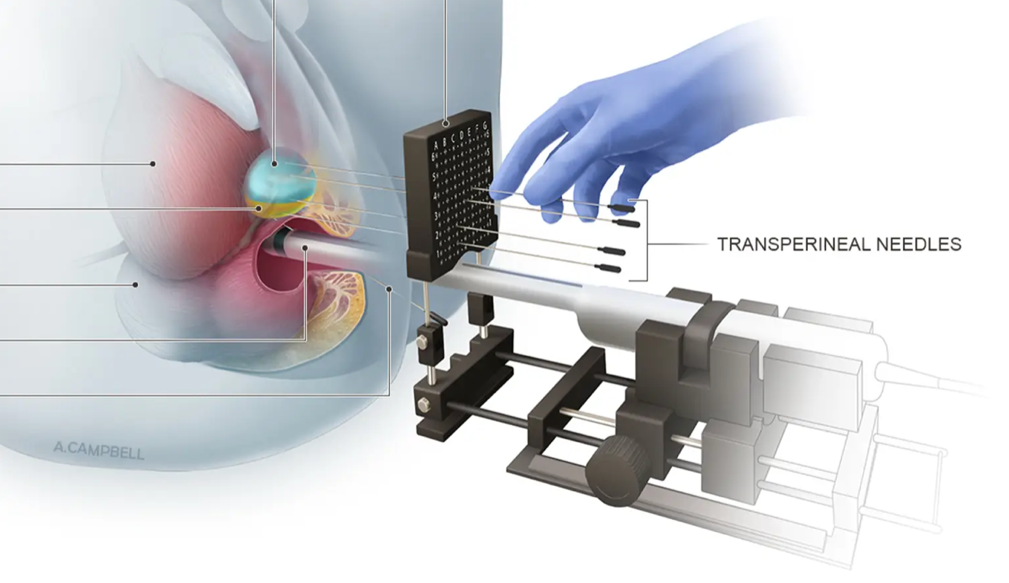
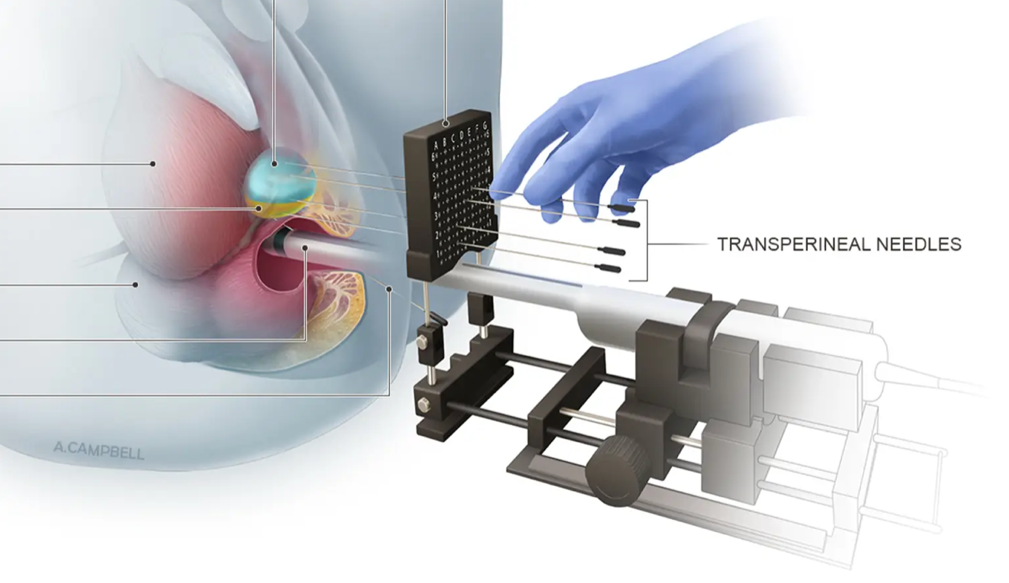
We offer two types of biopsy: the first is performed under local anaesthesia in the Urology Clinic, and the second performed under general anaesthesia in the operating theatre. The urologist will evaluate several factors, including prostate size, tumour size and the patient’s overall health, to determine the most suitable biopsy approach for the situation.
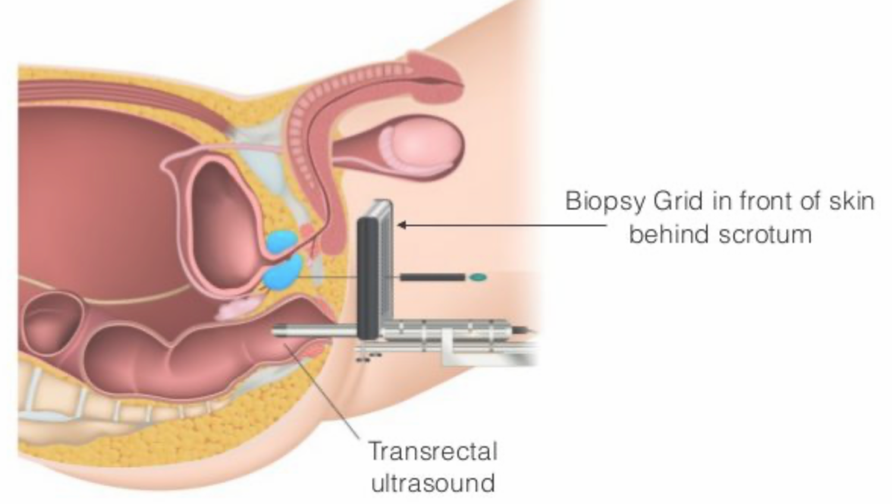
During a trans-perineal biopsy, the doctor will insert a lubricated ultrasound probe into the rectum to visualise the prostate. Local anaesthetic will be administered to numb the biopsy area, followed by the insertion of the biopsy needle through the skin between the testicles and the rectum. We use the trans-perineal biopsy technique, as opposed to the older technique (trans-rectal biopsy) which involves the biopsy needle passing through the rectum. The newer technique minimises the risk of serious infections.
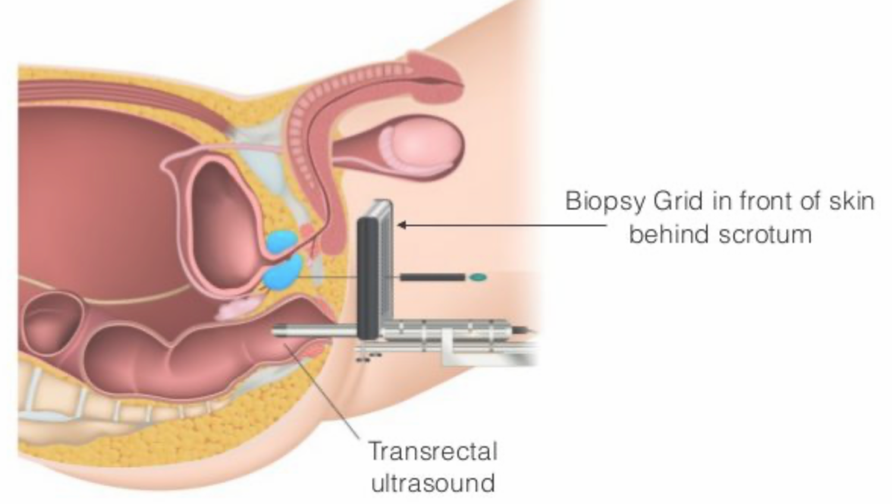
MRI/Ultrasound Fusion technology enables the use of MRI images to target specific abnormal areas identified by a radiologist. The urologist will have access to MRI images highlighting suspicious areas marked out. These images are then fused with real-time transrectal ultrasound images of the prostate. This fusion allows for the targeted sampling of suspicious areas, guided by ultrasound. The biopsy procedure is performed under general anaesthesia in the operating theatre.
We offer robotic radical prostatectomy as a treatment for localised or locally advanced prostate cancer. This minimally invasive surgery uses surgical robotic equipment to remove the entire prostate. The robotic laparoscopic technique allows surgeons to operate through small ports rather than large incisions. Surgical robotics seamlessly integrates minimally invasive techniques with advanced clinical technology.
The three-dimensional vision system magnifies the surgical field, improving the surgeon’s ability to recognise and control small blood vessels. Because of robotic technology, surgeons can perform minimally invasive procedures with higher precision, leading to shorter recovery times, reduced blood loss and shorter hospital stays.

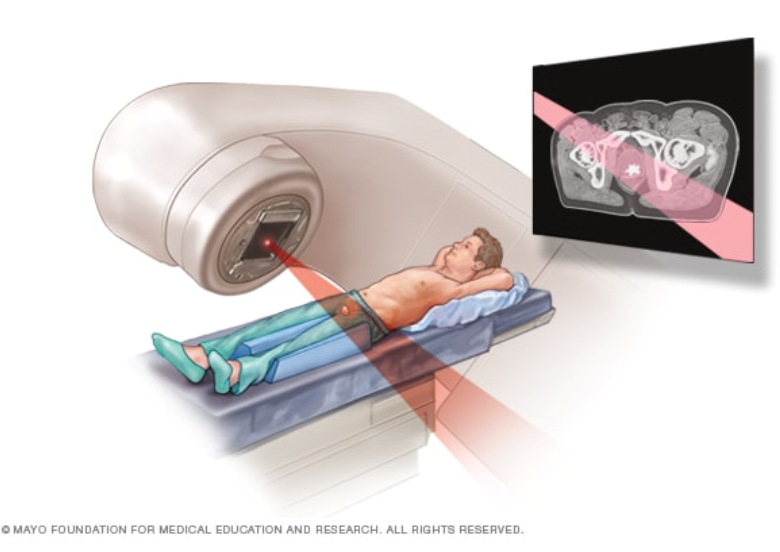
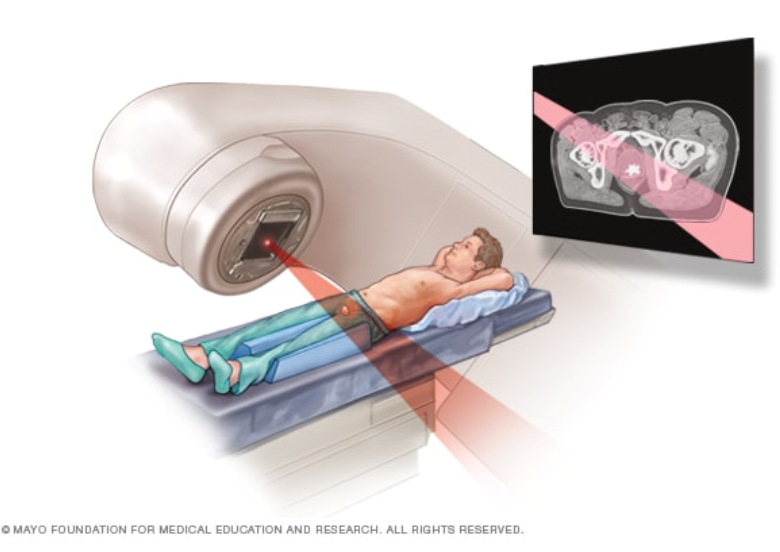
Beams of radiation are directed at the prostate gland from a machine outside the body. This type of radiation can be used to treat localised or locally advanced prostate cancer. Treatments are administered five days a week in an outpatient centre over several weeks. Each session is painless, similar to receiving an X-ray but with a higher dose of radiation. We offer radiotherapy as an alternative to robotic prostatectomy. The urologist will assist you in making an informed decision between radiotherapy and robotic prostatectomy, considering factors such as the extent of the disease and the patient’s overall health.