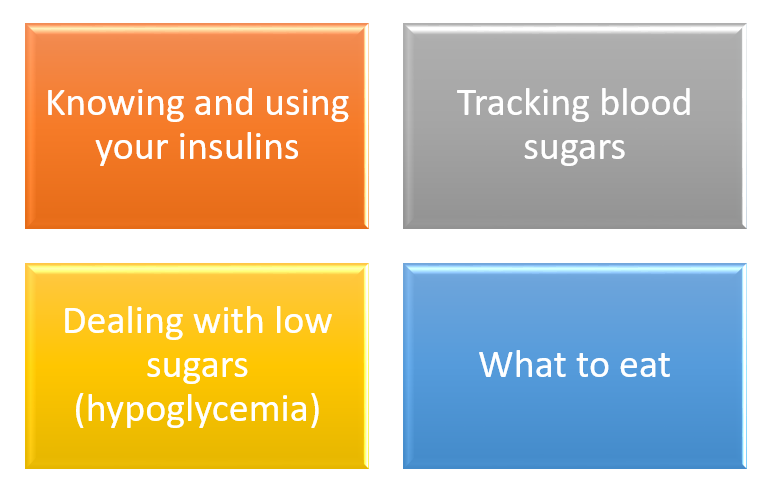
It is common to feel overwhelmed initially when learning new skills. Focus on these basic skills first.
Like learning something new for the first time, it's normal not to master everything immediately. Allow yourself time to adapt and improve through practice.
1. Knowing and using your insulins
Because your body is unable to produce insulin, it needs to administered through injections. You will be prescribed with two types of insulin:
- Basal insulin: A long-acting insulin, administered once or twice daily
- Quick-acting insulin: Administered before each meal
Self-injection might seem daunting initially. For a practical guide on insulin injection and tips for a less painful experience, click here.
2. Monitoring blood sugar levels
Regularly checking your blood sugar levels helps you understand your body better and also enables your healthcare team to offer more effective support. It will take some time to stabilise your blood sugar levels, please remain patient during this process.
Learn about glucose monitoring here.
3. Managing hypoglycaemia (low blood sugar)
Your blood sugar might drop below 4 mmol/L due to an imbalance between your insulin dose and food intake, or due to other factors like physical activity. Learn how to manage low blood glucose effectively with this quick reference.
4. What to eat
Step 1: Healthy eating and reducing sugar intake
Begin by focusing on healthy eating habits and minimising sugar intake. Avoid simple sugars like those in sugar-sweetened beverages and sweets to reduce large spikes in blood sugar levels.
Step 2: Identifying carbohydrates and practicing portion control
As you monitor your blood sugar levels, you may begin to notice that the more carbohydrates you consume, the higher the blood sugar levels will rise. Carbohydrates are found in foods like rice, noodles, root vegetables (e.g. potatoes), bread and sugary foods or drinks.
You may also observe blood sugar levels dropping to hypoglycaemia levels (<4 mmol/L) after eating, if you eat too little carbohydrates.
Therefore, recognizing carbohydrates and practicing portion control can help you keep your blood sugar levels within target range. For more information on carbohydrates and food label reading, visit Diabetes and Food.
Step 3: Learning carbohydrate counting
As you become more adept, consult your healthcare team about learning carbohydrate counting and adjusting meal-time insulin doses based on what you plan to eat. This will enable you to eat a variety of meals more confidently. A dietitian can provide tailored guidance to enhance your confidence in managing a diverse diet.