A liver biopsy involves removing a small sample of liver tissue for microscopic examination. This is typically done using a needle inserted into the liver to extract a tissue sample for analysis.
Why do I need to have a liver biopsy?
A liver biopsy assists doctors in diagnosing specific liver conditions and determining their severity, which is vital for guiding treatment. Your doctor will discuss in detail the reasons for the biopsy prior to the procedure.
Are there complications to doing a liver biopsy?
While liver biopsies are generally safe, some complications may occur. These include:
- Fleeting discomfort in the right side or shoulder, usually manageable with painkillers and resolving quickly.
- Severe pain (2%)
- Bleeding (0.3 – 0.5%)
- Puncture of other organs (0.01-0.1%)
These complications are rare and typically managed without surgery. However, in very rare cases, complications from a liver biopsy can lead to surgery or even death.
How is a liver biopsy performed?
Liver biopsies can be performed either bedside by a liver specialist or under ultrasound guidance by a radiologist. Typically, this outpatient procedure takes place in the day surgery ward.
During the biopsy, you will lie on your back while a specific skin area is targeted with ultrasound assistance. After cleaning the area, a local anaesthetic is applied to numb the skin and underlying tissue. The doctor will guide your breathing, instructing when to hold your breath. At this moment, a thin needle is inserted through the skin into the liver, quickly extracting a tissue sample. The process takes only one to two seconds. To ensure comfort, medication may be administered. The extracted tissue is then sent for laboratory analysis. The entire procedure lasts approximately 15 to 20 minutes.
What will I expect on the day?
On the day of the biopsy, you will be admitted to the day surgery ward in the morning. Blood tests may be conducted to ensure the safety of the procedure. After undergoing the liver biopsy, as described, you will be monitored in the ward for four to six hours. During this period, nurses will check your blood pressure, heart rate and manage any pain with painkillers. A doctor will review and examine you before discharge. The total duration from admission to discharge can be up to eight hours.
Will there be serious damage to my liver?
As the biopsy involves removing only a small piece of liver tissue, it does not cause significant damage to the liver.
What do I need to watch out for?
Post-procedure, patients should avoid strenuous physical activity and lifting heavy weights for two weeks. A medical certificate for rest will be issued. If you experience faintness, blackouts, palpitations or severe pain after returning home, seek immediate medical attention.
Are there any other alternative approaches to a liver biopsy?
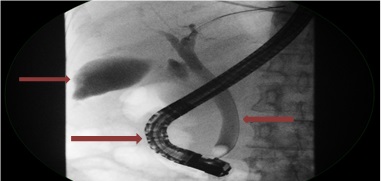
An alternative method is the transjugular liver biopsy, involving a needle passed through a tube in a neck vein, extracting liver tissue through the blood vessel. This method poses an even lower risk of bleeding and is safer for patients with abnormal blood clotting. However, it may yield less diagnostic tissue and is more costly. This approach may be recommended for patients with a high risk of bleeding.
For any questions about liver biopsy, please contact one of our hepatologists.
For information on other specialist endoscopic procedures and motility and functional investigations, please click here.