Basal insulin provides a consistent background level of insulin to stabilise blood glucose levels throughout the day, including periods of fasting.
Even when you are not eating, your body requires a small amount of basal insulin to keep blood glucose levels from rising.
This insulin type is generally injected once or twice daily, due to its longer duration of action compared to quick-acting insulin.
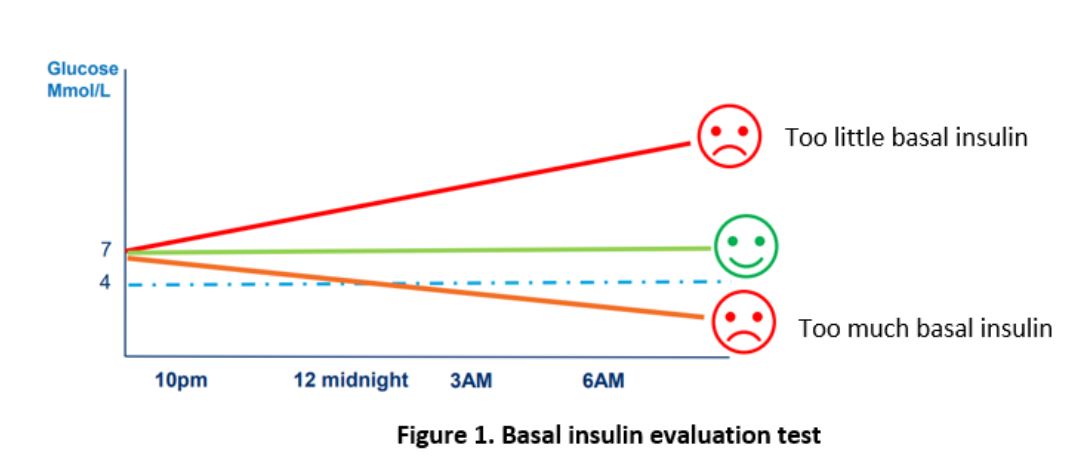
The dose of basal insulin is usually 40 to 50% of your total daily insulin dose. Too little basal insulin can cause high blood glucose. Too much basal insulin can cause hypoglycaemia especially when you miss a meal or when you sleep. Being on the right dose will keep your glucose levels stable when you are not eating (Figure 1).
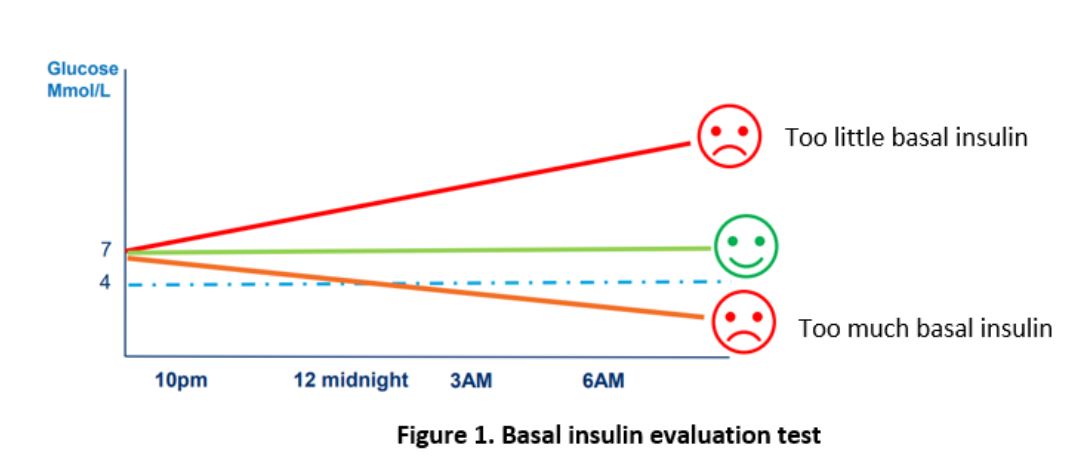
Utilise this worksheet (Overnight basal insulin evaluation worksheet) under the guidance of your healthcare team to assess if your basal insulin dose is appropriate.